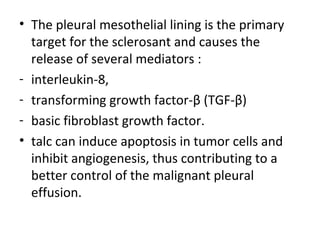
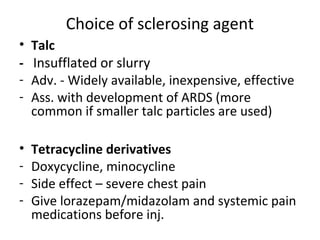
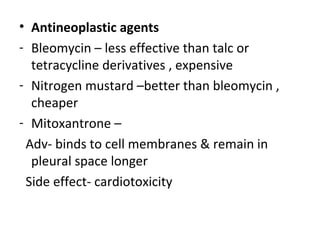
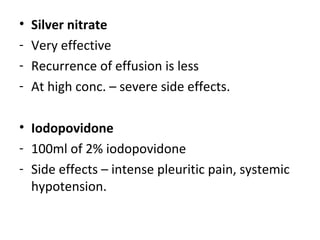
Pleurodesis is a procedure to induce adhesion of the pleural layers to treat recurrent pneumothorax or malignant pleural effusion. It involves using sclerosing agents or surgical abrasion. Talc, tetracycline derivatives like doxycycline, and minocycline are common sclerosing agents used. The procedure involves draining the pleural fluid then injecting the sclerosing agent through a chest tube while the lung is expanded to cause an inflammatory response and formation of fibrous adhesions between the pleural layers.