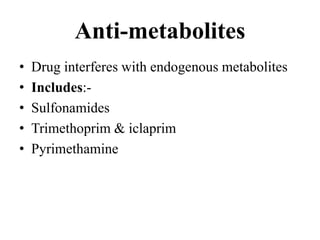
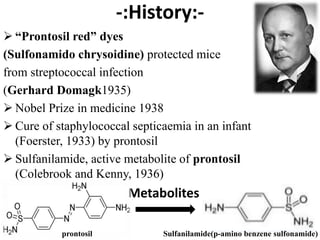
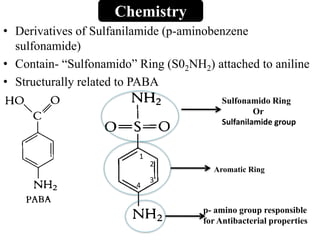
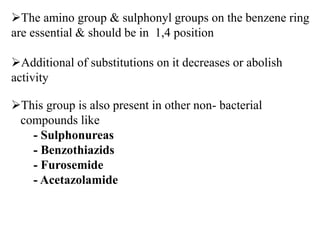
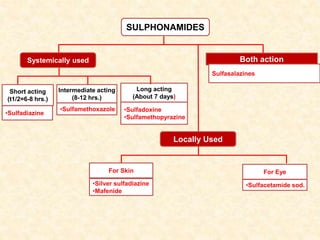
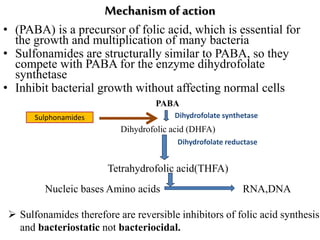
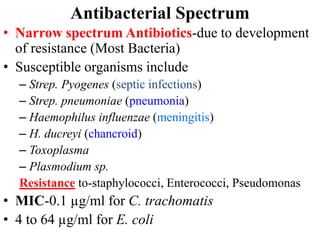
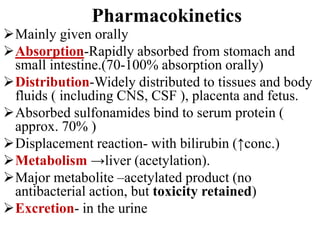
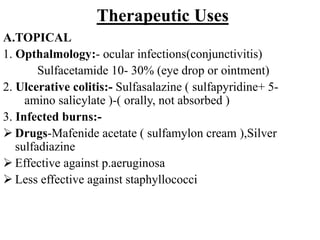
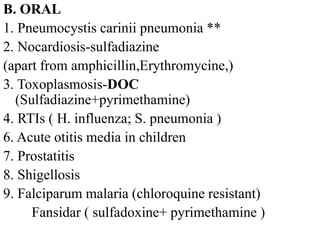
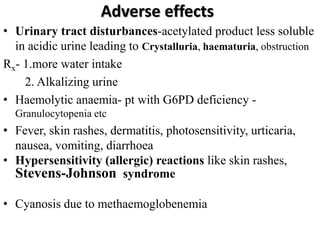
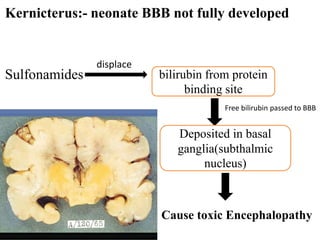
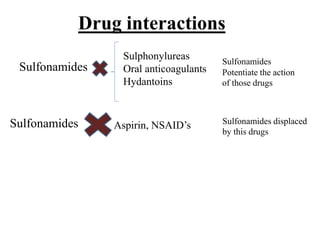
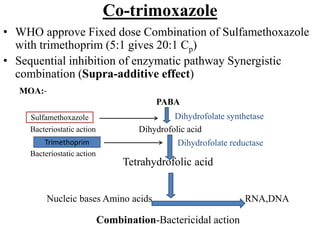
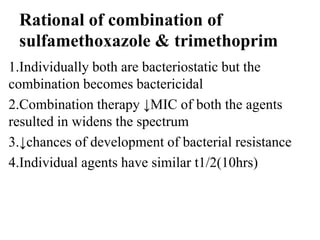
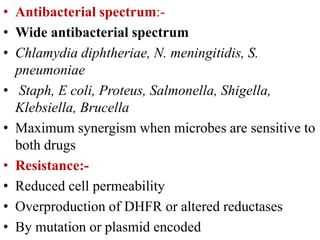
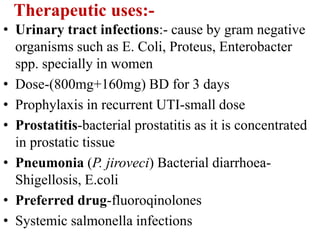
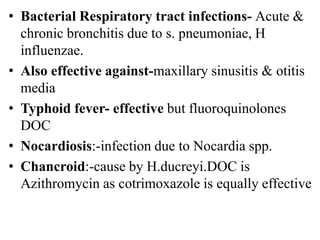
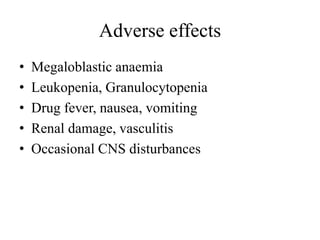
This document discusses sulfonamides, including their history, mechanism of action, uses, and adverse effects. It notes that sulfonamides were the first synthetic antibacterial agents and are bacteriostatic, inhibiting bacterial synthesis of folic acid. Co-trimoxazole is a fixed dose combination of sulfamethoxazole and trimethoprim that has a synergistic effect. The combination is widely used to treat urinary tract infections, pneumonia, and travelers' diarrhea. Common adverse effects include rashes, nausea, and hematologic issues.