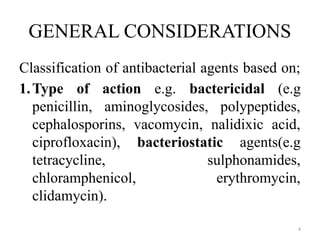
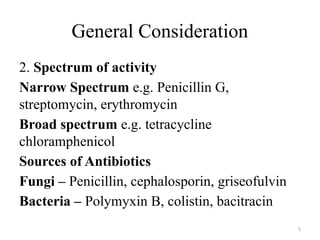
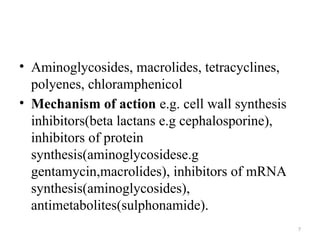
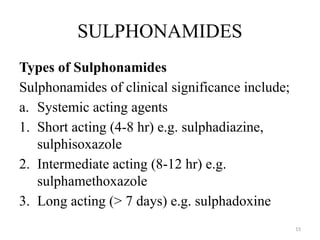
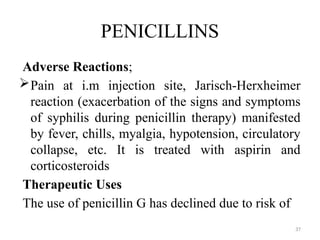
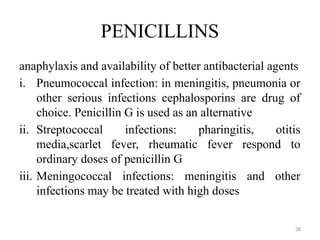
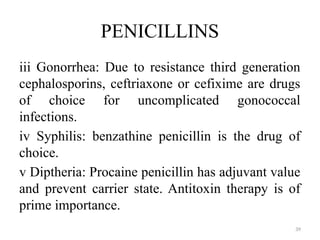
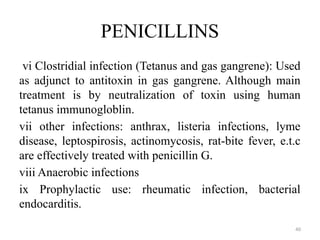
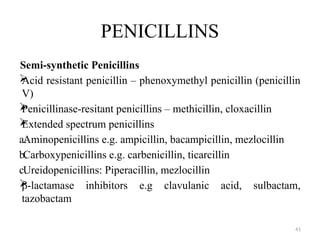
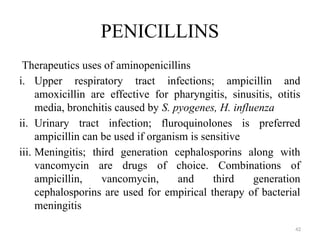
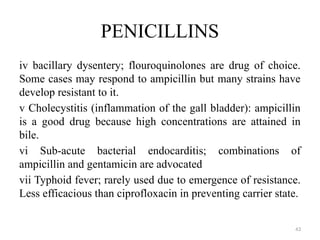
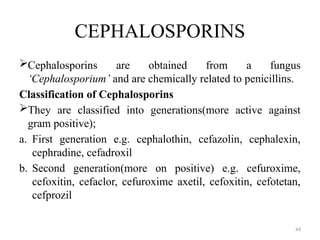
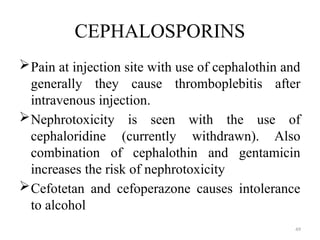
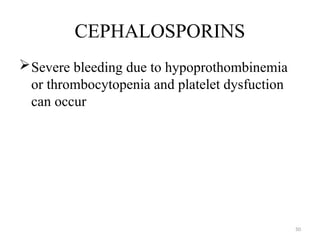
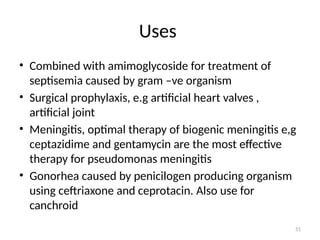
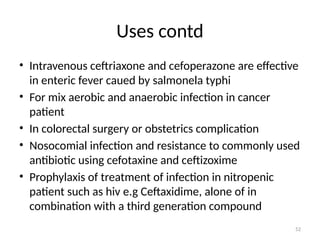
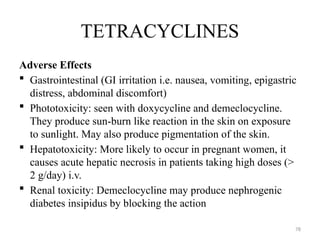
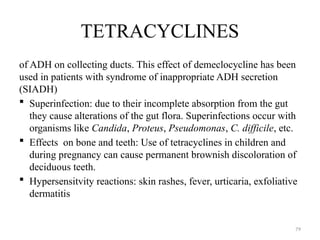
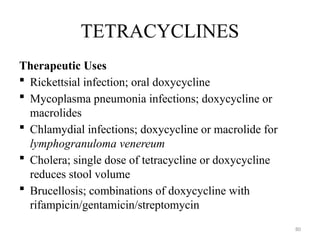
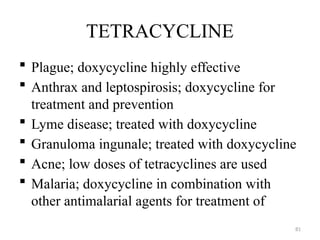
The document discusses anti-bacterial agents, specifically their classification, mechanisms of action, and therapeutic uses. It highlights the limitations such as drug resistance, toxicity, and potential for superinfections, along with the advantages of combining antimicrobial agents. Additionally, specific classes of antibiotics like sulphonamides and penicillins are detailed regarding their mechanisms, pharmacokinetics, and adverse effects.