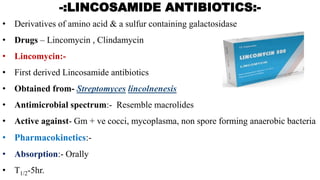
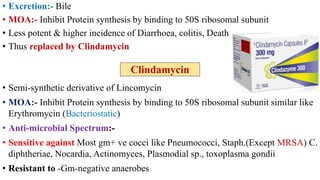
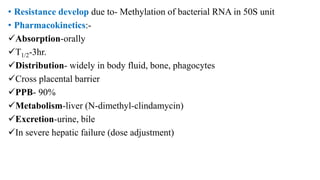
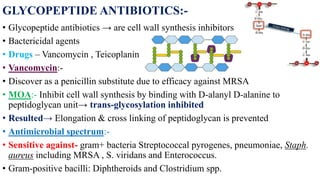
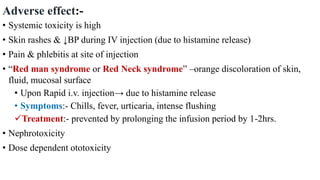
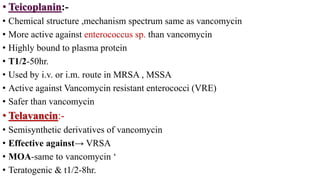
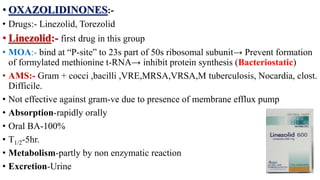
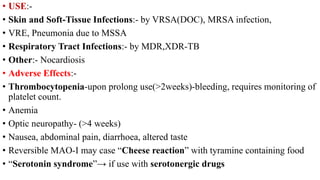
This document summarizes various classes of antimicrobials including lincosamide antibiotics, glycopeptide antibiotics, oxazolidinones, polypeptide antibiotics, and urinary antiseptics. It describes the mechanism of action, antimicrobial spectrum, pharmacokinetics, uses, and adverse effects of lincomycin, clindamycin, vancomycin, teicoplanin, linezolid, polymyxin B, colistin, bacitracin, nitrofurantoin, and methenamine. It also discusses the treatment of lower urinary tract infections with these urinary antiseptics and other antimicrobials like cotrimoxazole, quinolones