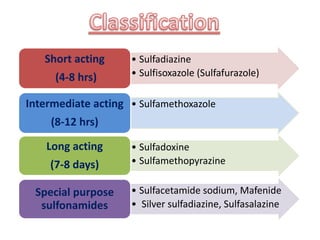
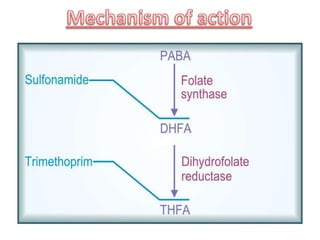
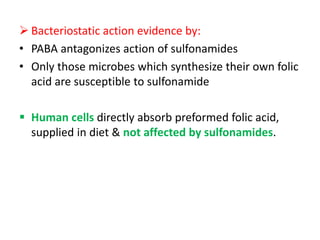
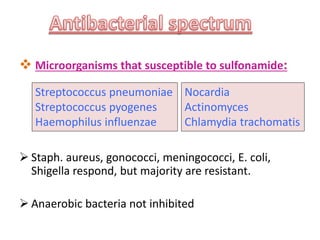
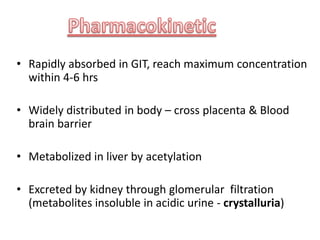
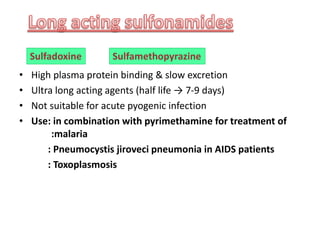
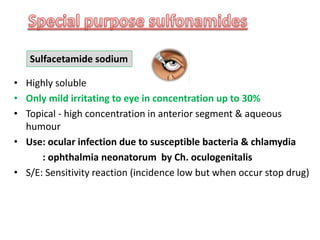
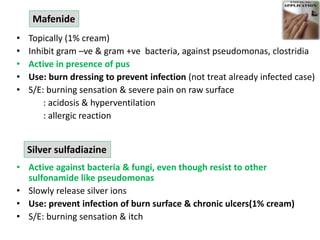
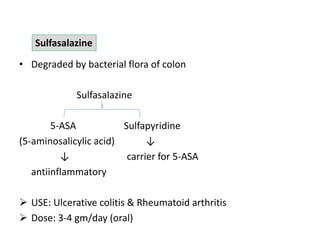
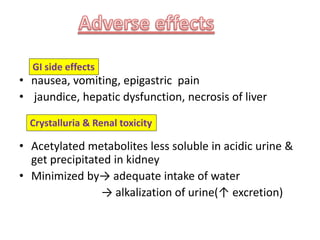
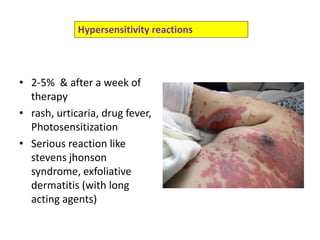
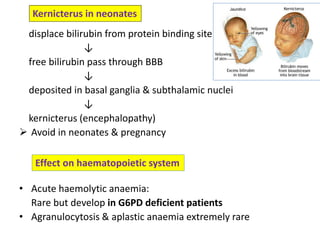
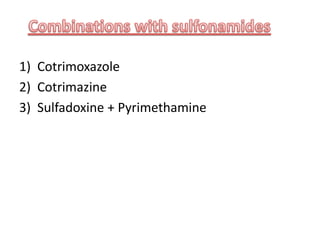
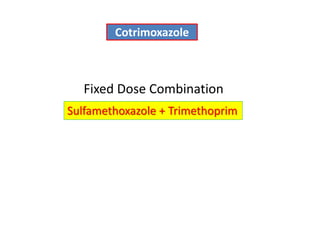
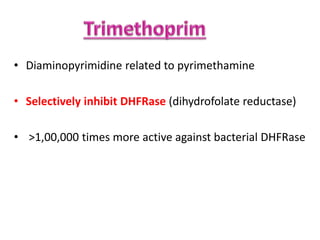
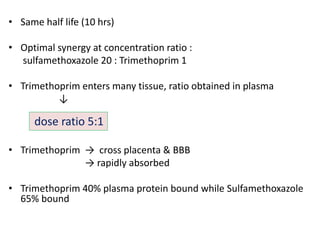
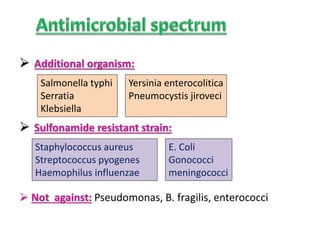
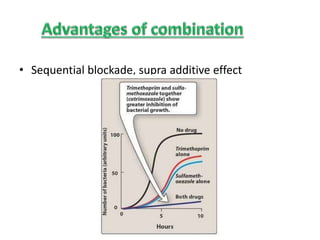
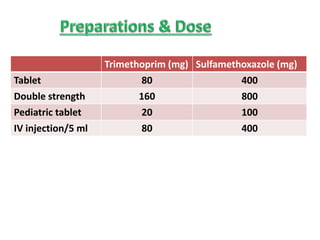
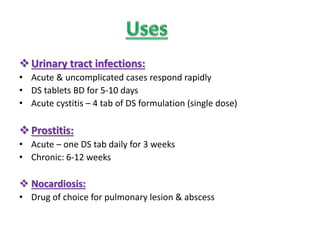
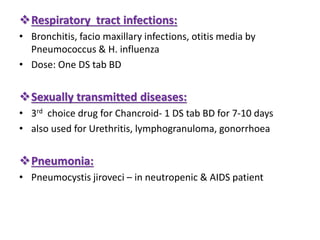
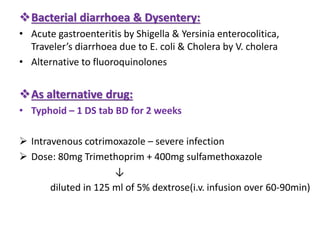
This document discusses sulfonamide antibiotics. It provides information on different types of sulfonamides including short, intermediate and long acting agents. It describes their mechanisms of action, antimicrobial spectrum, pharmacokinetics, uses, and side effects. It also discusses fixed dose combinations like cotrimoxazole and its uses for various infections.

![ Sulfonamide: Sulfone + amide
Sulfanilamide [p-aminobenzene sulfonamide]](https://image.slidesharecdn.com/sulfonamide-210806055449/85/Sulfonamide-3-320.jpg)




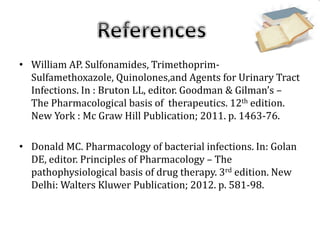
![• Tripathi KD. Essentials of Medical Pharmacology. 6th ed. New
Delhi : Jaypee brothers medical publishers; 2009. p. 360-71.
• Sharma HL & Sharma KK. Principles of Pharmacology. 2nd ed.
New Delhi: Paras publication; 2012. p. 702-16.
• Casini A, Scozzafava A, Supuran LT. Sulfonamides and
sulfonylated derivatives as anticancer agents. Curr Cancer Drug
Targets.[Internet] 2002 [cited in 2014 June 30];2(1):55-75.
Available from: Medline](https://image.slidesharecdn.com/sulfonamide-210806055449/85/Sulfonamide-59-320.jpg)
