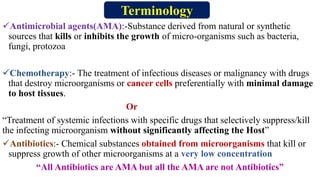
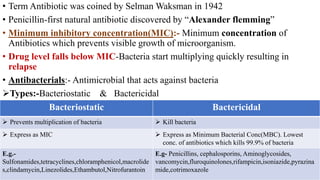
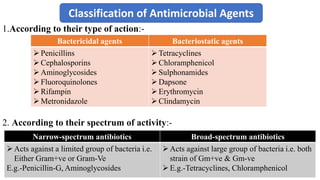
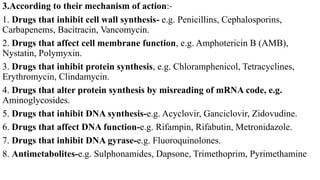
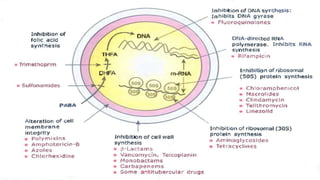
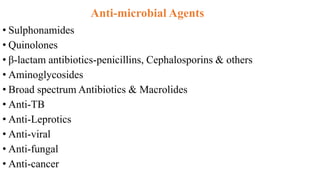
1. Antimicrobial agents include substances that kill or inhibit the growth of microorganisms such as bacteria, fungi, and protozoa. They are commonly classified based on their mechanism of action and spectrum of activity.
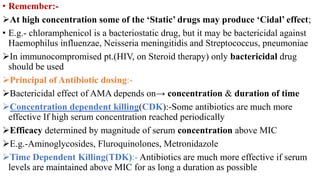
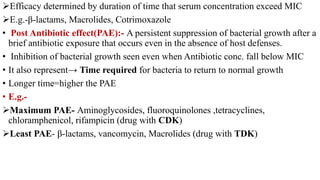
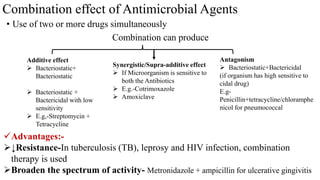
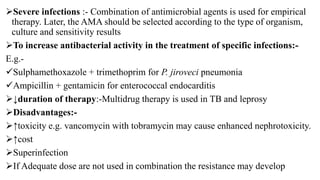
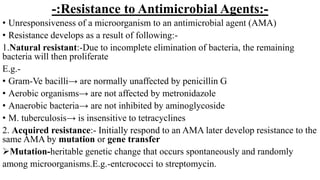
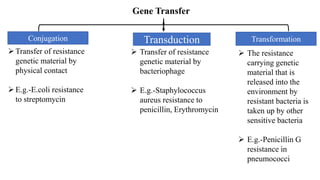
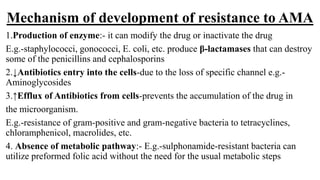
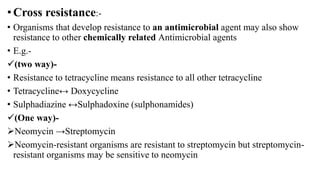
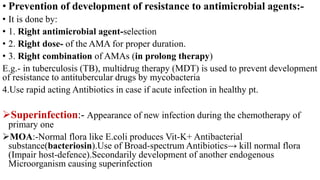
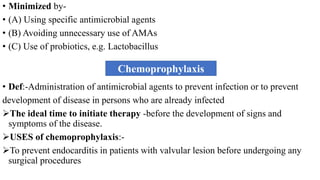
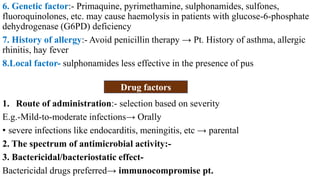
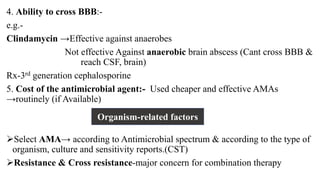
2. Antimicrobial resistance can develop through natural resistance, mutation, or gene transfer between microorganisms. It is important to select the right antimicrobial agent, use the proper dose for sufficient duration, and consider combination therapy to prevent resistance.
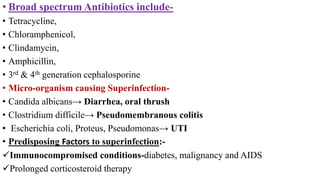
3. Superinfections can sometimes occur during antimicrobial therapy due to elimination of normal protective flora. Probiotics and prudent antimicrobial use can help reduce this risk.