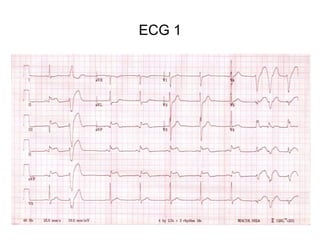
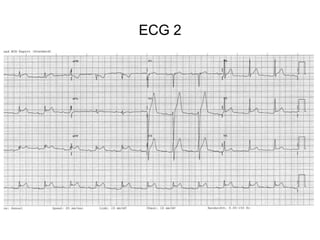
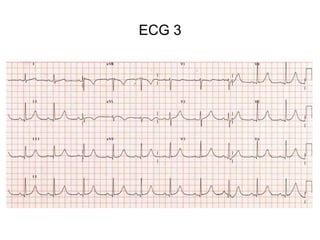
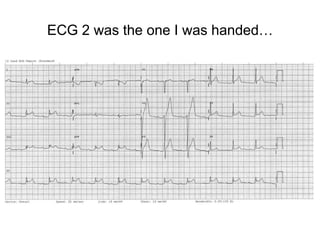
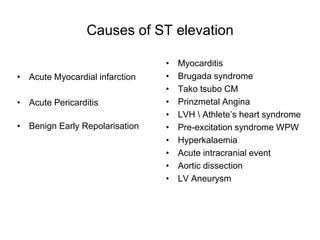
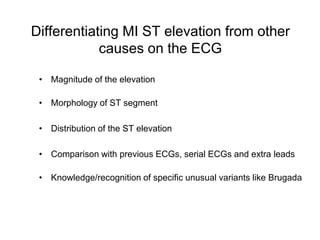
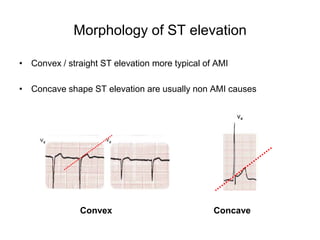
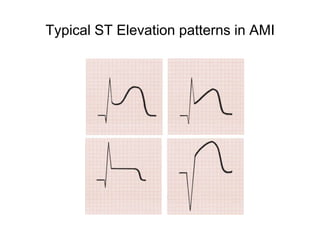
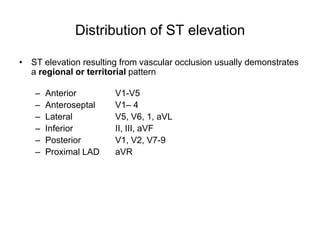
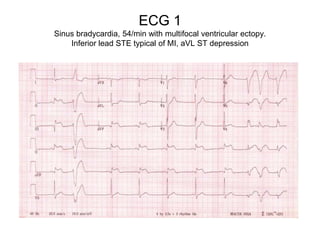
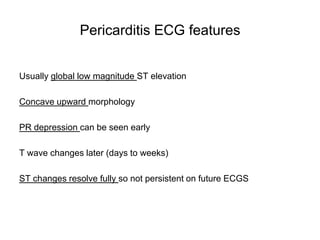
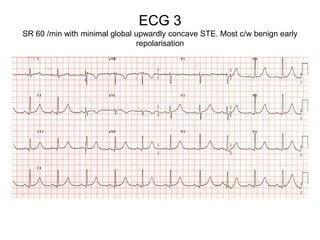
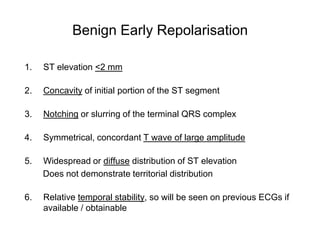
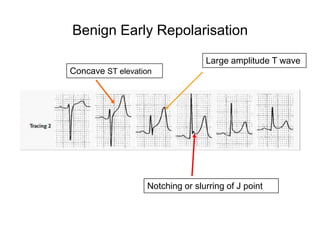
The document discusses differentiating ST elevation myocardial infarction (STEMI) from other causes of ST elevation on an electrocardiogram (ECG). It provides examples of three sample ECGs, describing ECG 1 as showing typical inferior STEMI patterns, ECG 2 as most consistent with pericarditis given its global and concave ST elevation, and ECG 3 showing minimal changes consistent with benign early repolarization. Key factors for differentiation include the magnitude, morphology, distribution of ST elevation, and comparison to previous ECGs. The document emphasizes analyzing ST elevation in the full clinical context and pursuing safe care when in doubt.