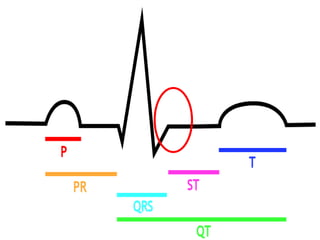
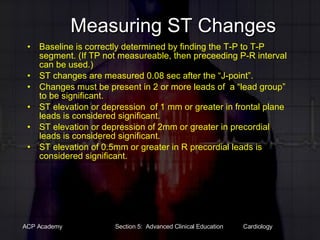
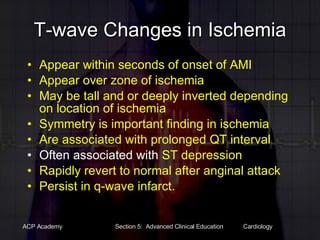
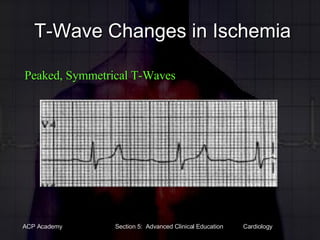
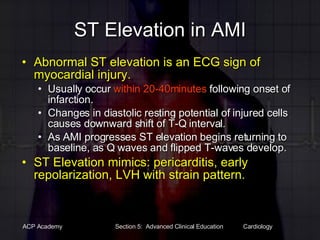
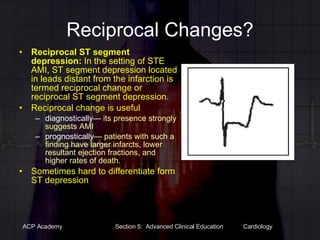
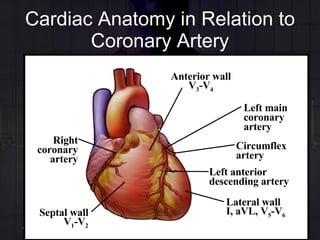
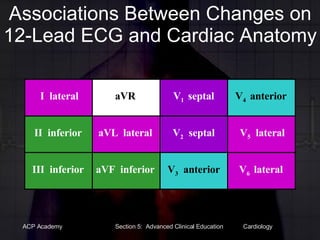
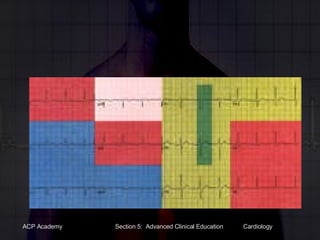
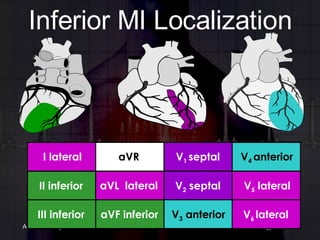
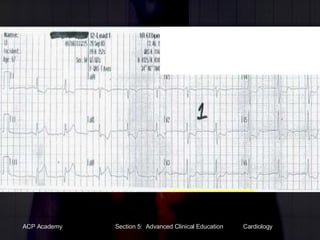
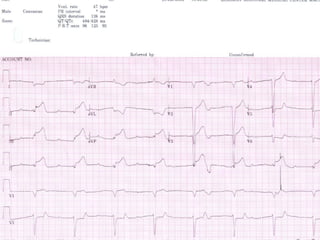
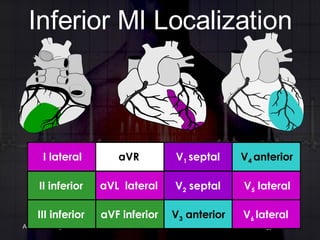
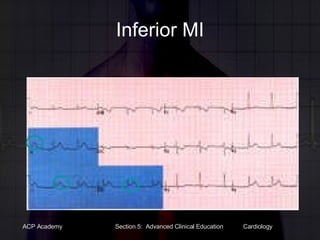
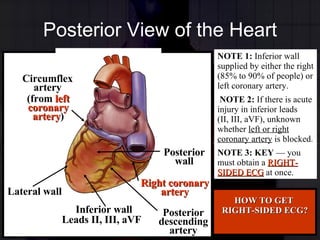
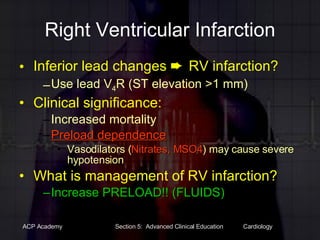
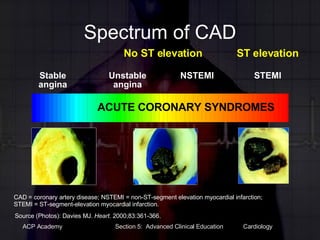
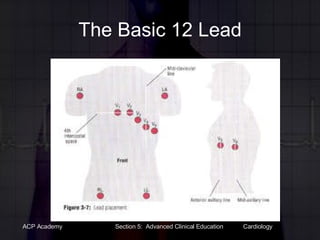
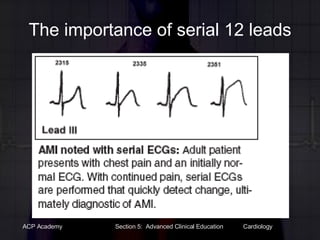
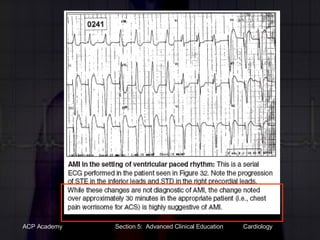
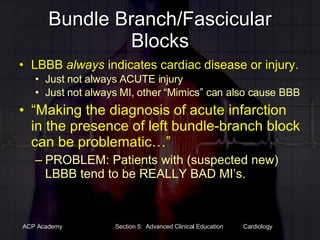
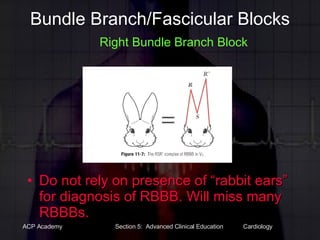
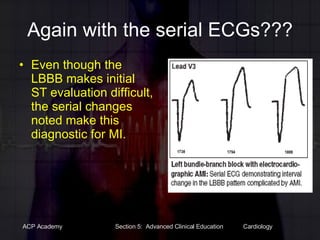
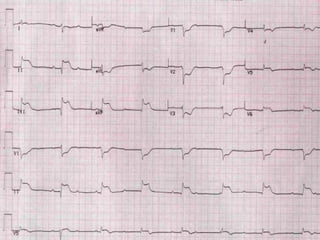
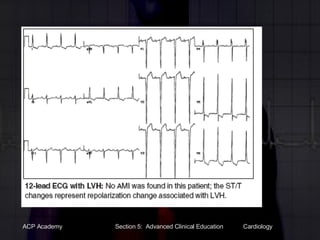
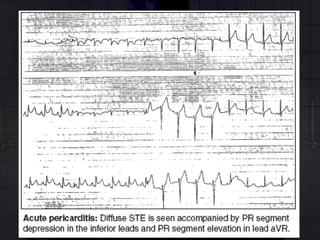
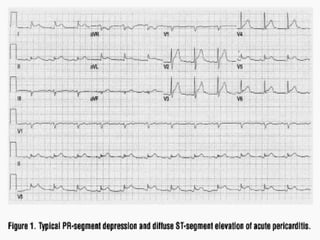
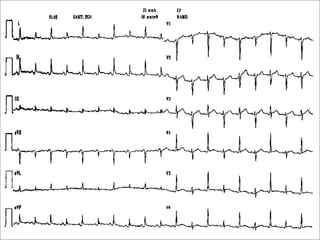
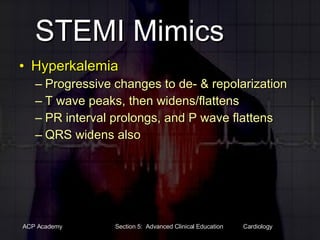
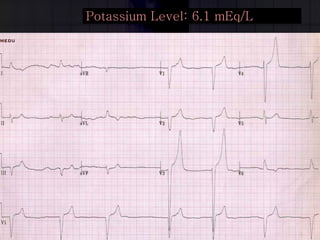
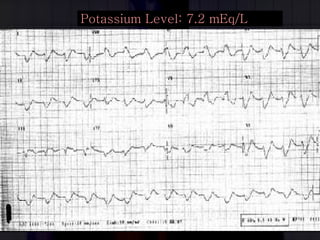
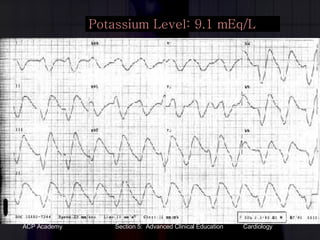
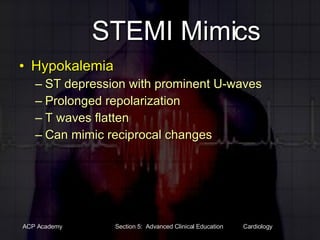
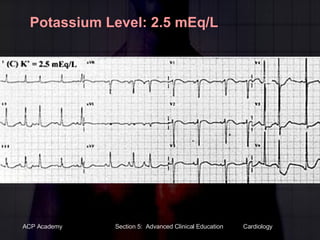
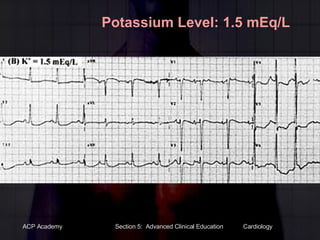
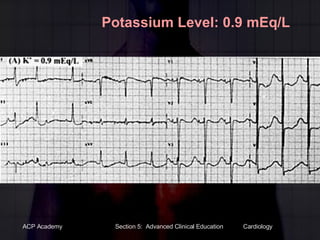
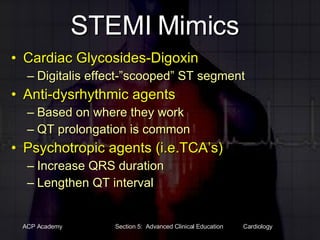
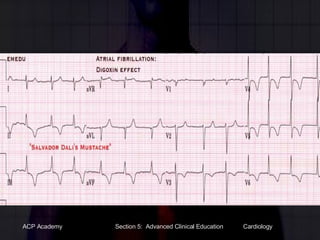
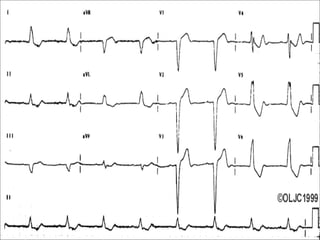
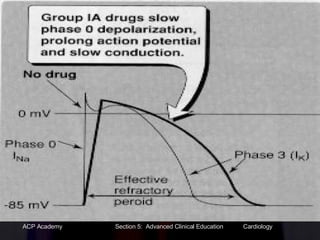
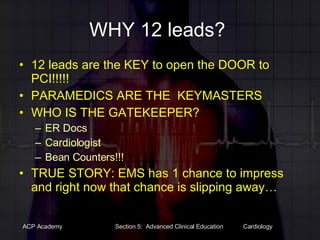
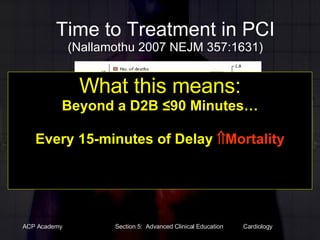
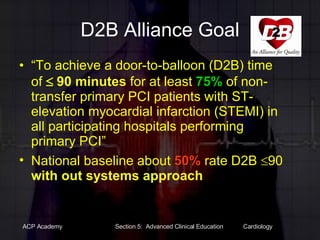
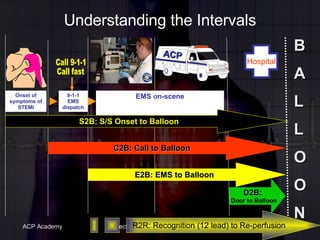
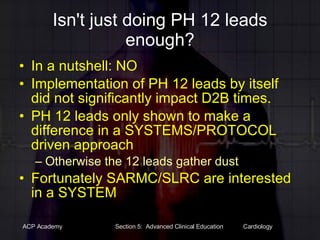
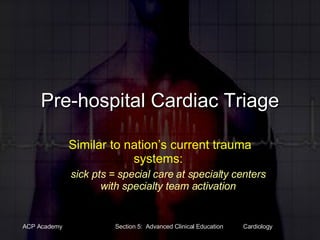
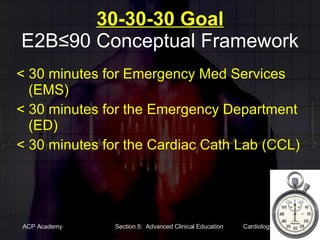
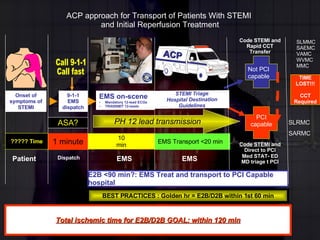
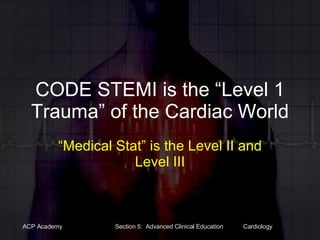
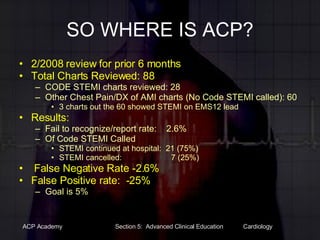
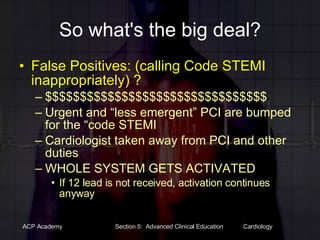
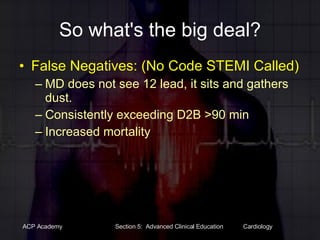
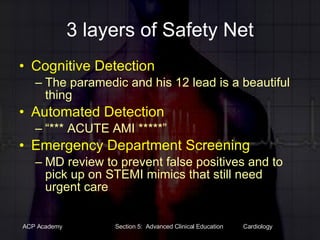
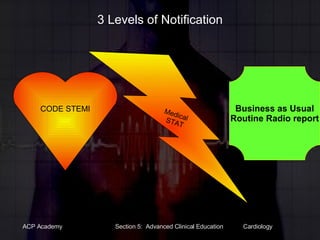
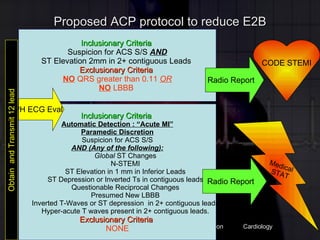
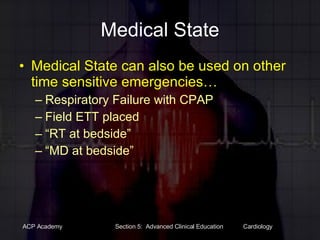
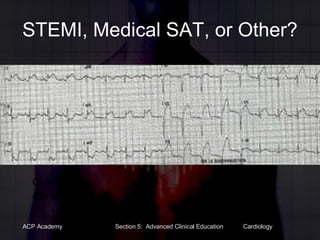
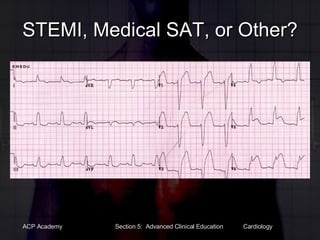
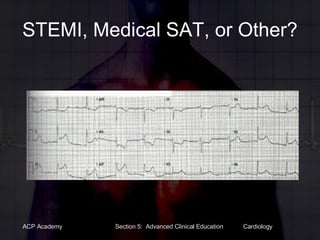
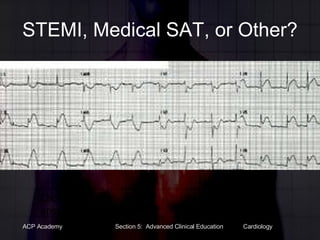
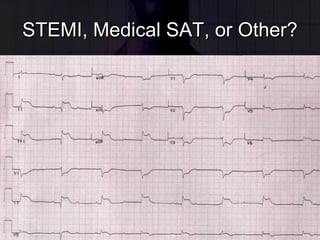
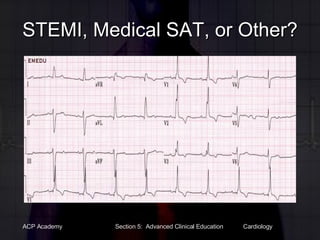
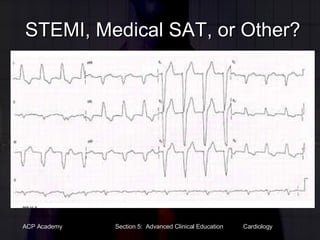
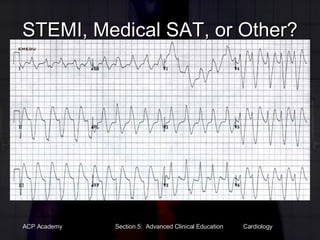
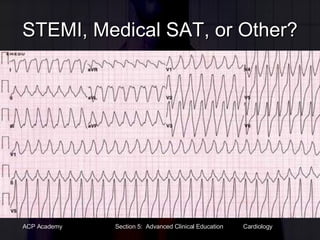
This document provides information on STEMI, NSTEMI, and STEMI mimics for paramedics. It discusses the importance of accurate 12-lead ECG interpretation for identifying STEMIs to reduce door-to-balloon times and improve outcomes. It outlines criteria for calling a "Code STEMI" to activate the cardiac catheterization lab as well as situations where a "Medical Stat" or routine transport would be more appropriate based on the 12-lead findings. The goal is to minimize false STEMI activations while still rapidly identifying true STEMIs.