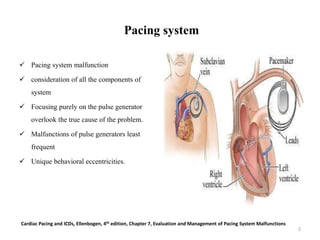
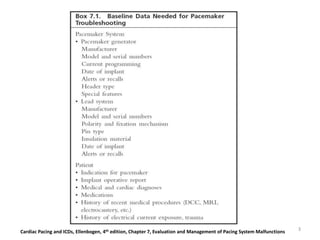
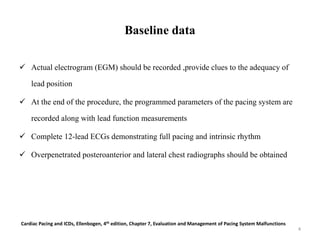
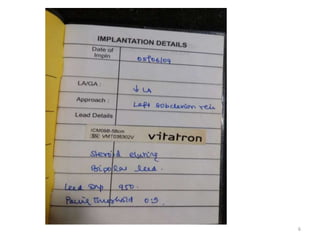
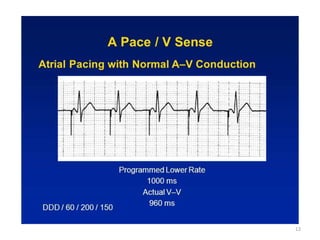
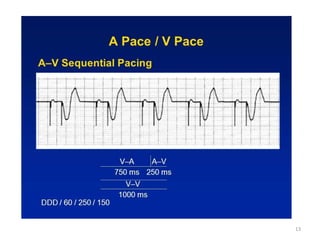
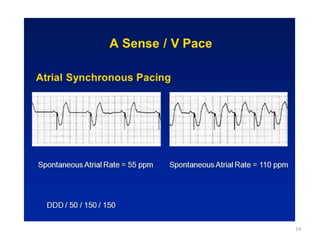
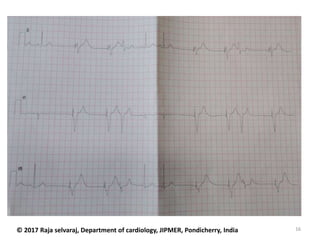
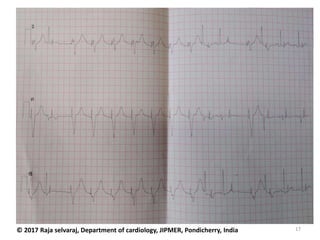
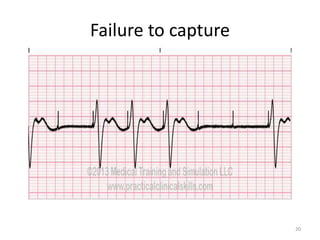
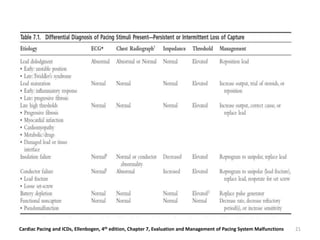
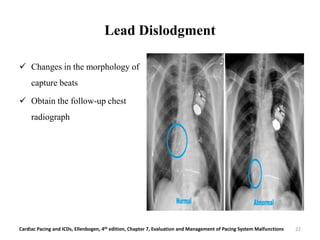
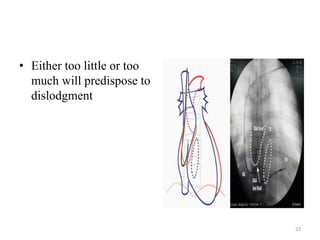
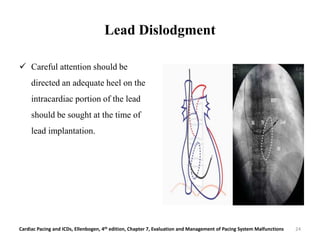
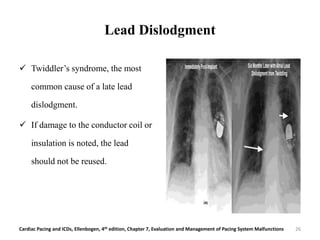
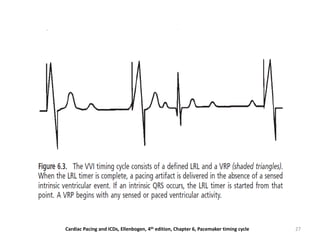
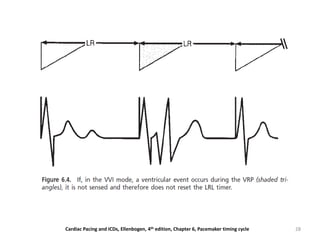
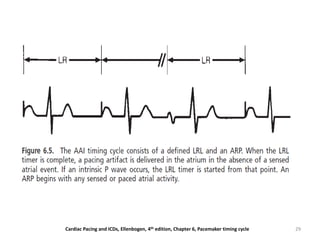
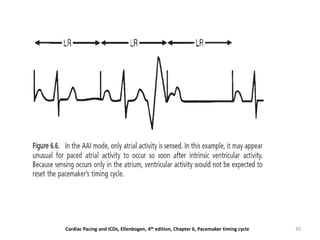
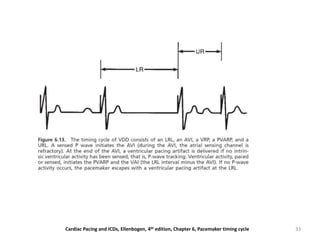
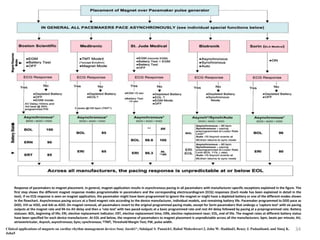
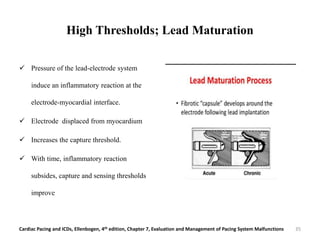
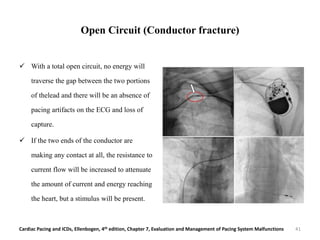
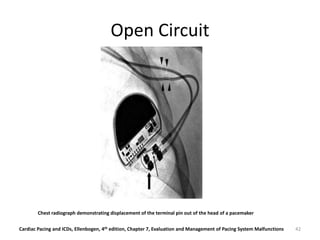
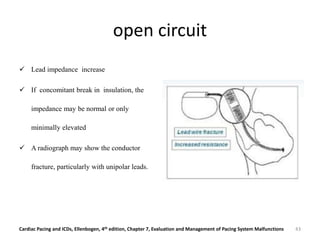
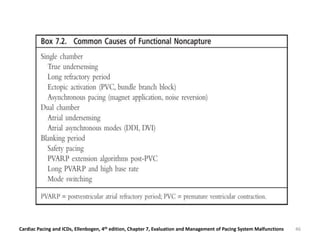
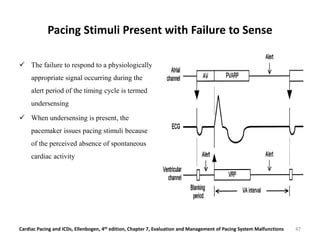
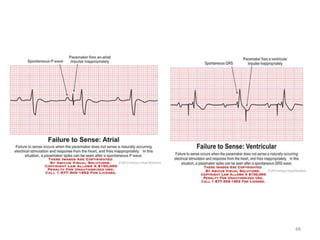
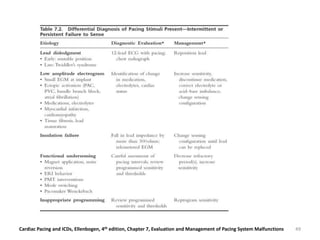
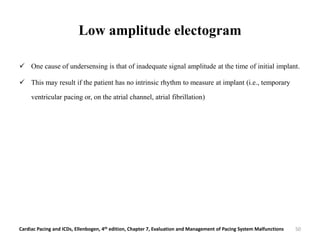
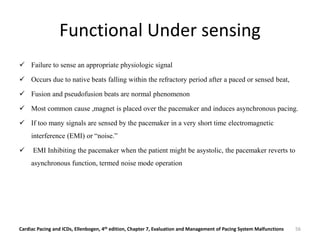
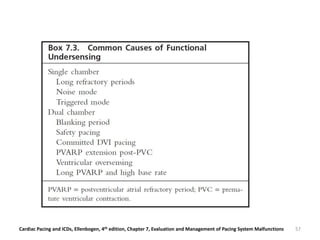
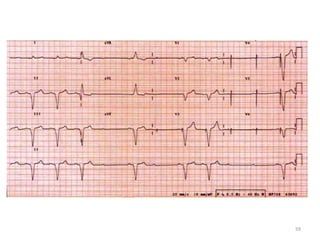
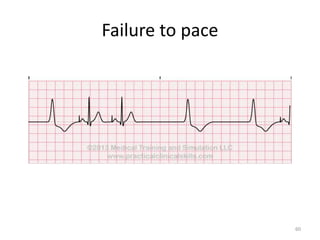
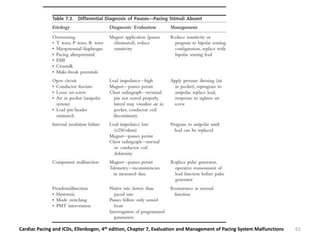
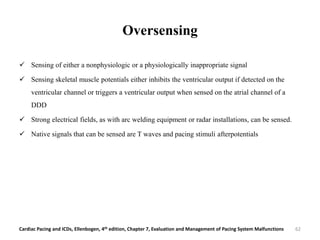
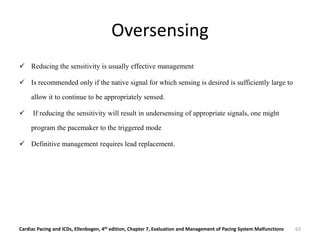
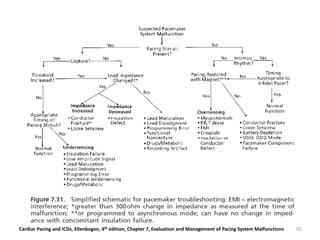
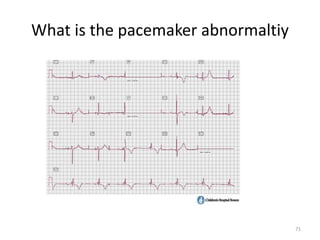
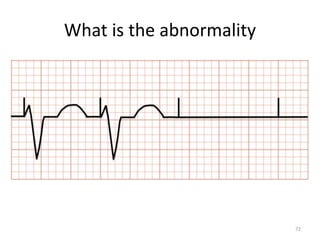
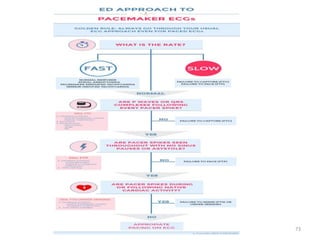
The document discusses the evaluation and management of pacemaker malfunctions. It describes how to differentiate between various types of single chamber pacemaker malfunctions including pacing stimuli present with failure to capture, pacing stimuli present with failure to sense, and pacing stimuli absent. Common causes of these malfunctions are then outlined such as lead dislodgment, insulation defects, threshold increases, and undersensing. The document stresses the importance of obtaining baseline pacemaker data during initial programming and follow-up to properly diagnose malfunctions.