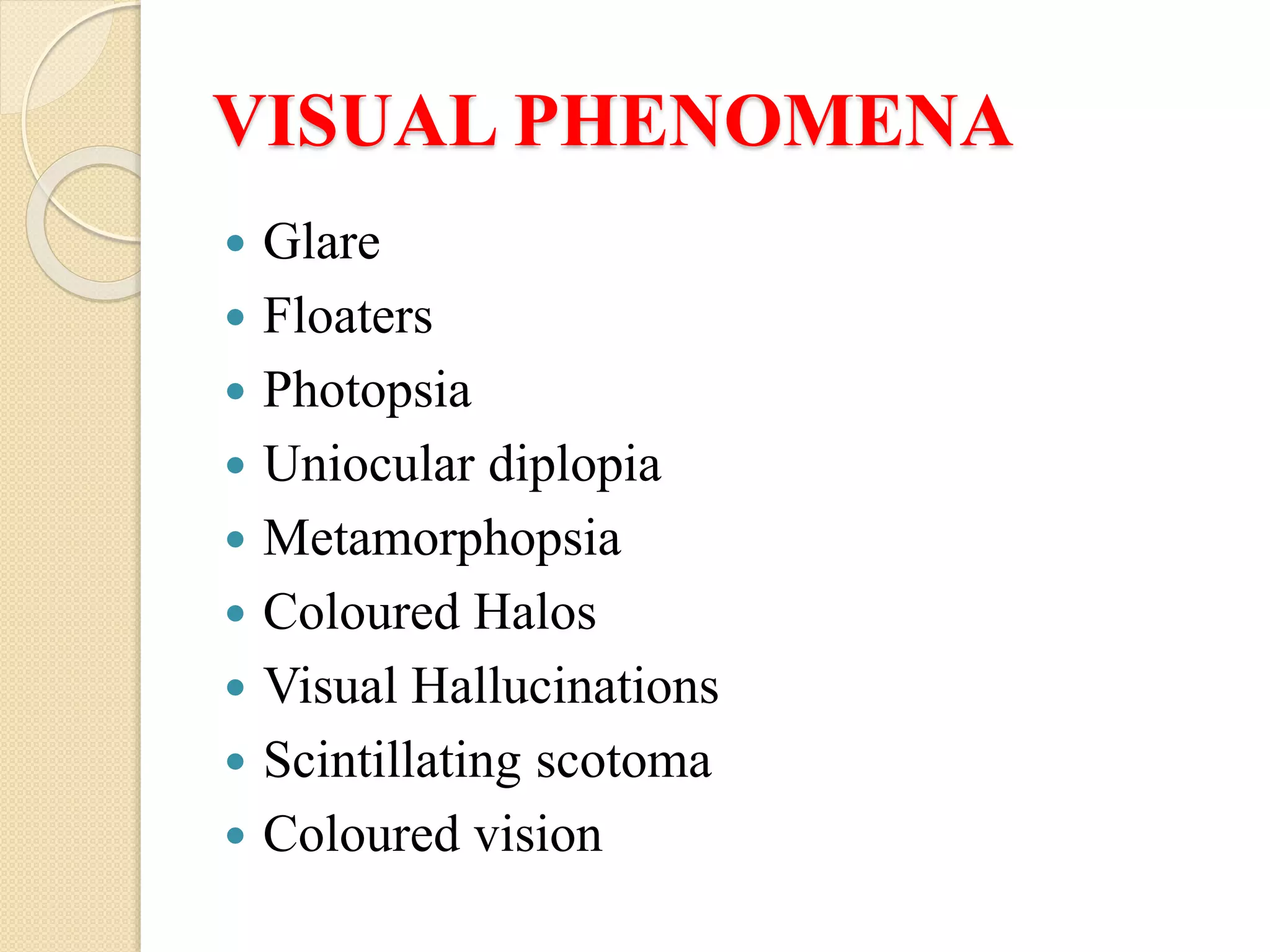
This document summarizes various ocular symptoms and their causes. It discusses anomalies of ocular motility such as asthenopia and binocular diplopia which can result from extraocular muscle imbalances or uncorrected refractive errors. It also describes disorders of the ocular surface including irritation, lacrimation, photophobia, and red eye which can be caused by dry eye, infections, or inflammation. Various visual phenomena like glare, floaters, photopsia, and others and their associations with conditions like vitreous degeneration, retinal tears, and migraines are outlined. Finally, it discusses diminution of vision including amblyopia, amaurosis, and their exogenous and bilateral causes like tox