This document provides information on rhegmatogenous retinal detachment including:
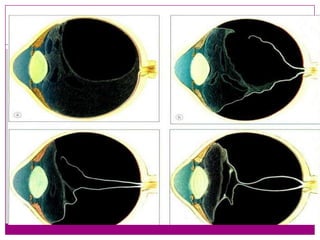
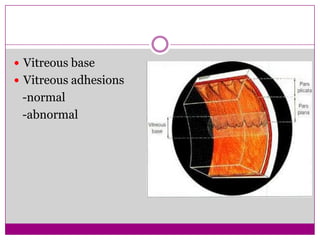
- The pathogenesis which involves vitreoretinal traction from liquefaction of the vitreous gel creating a hole that allows fluid into the subretinal space.
- Symptoms include photopsia, floaters, and visual field defects.
- Signs include Marcus Gunn pupil, low intraocular pressure, retinal breaks, and mild iritis.
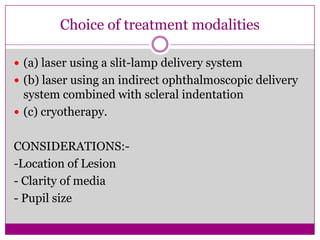
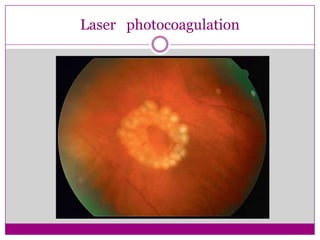
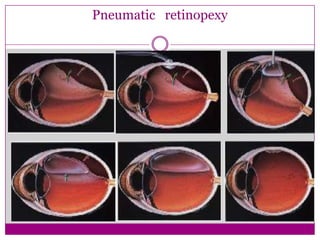
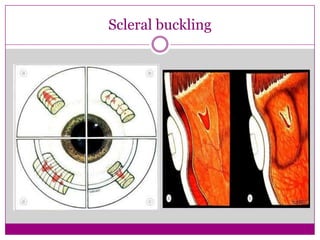
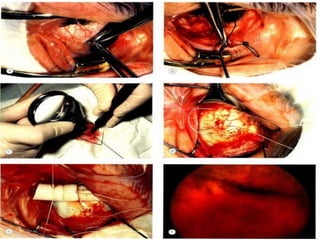
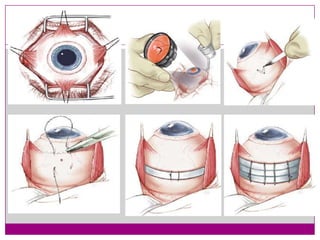
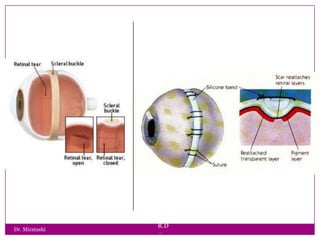
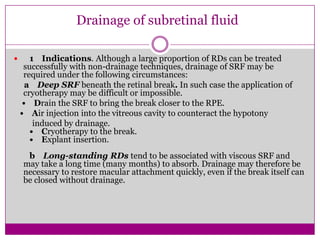
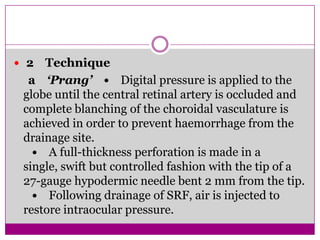
- Treatment options depend on factors like location and size of retinal break, state of vitreous gel, and include laser photocoagulation, cryotherapy, scleral buckling, pneumatic retinopexy, and drainage of subretinal fluid in




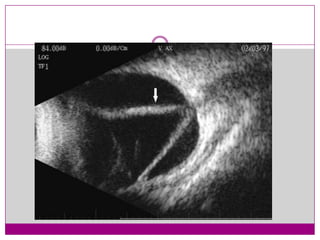
![Signs:
Marcus gunn pupil
Low IOP relative
‘Tobacco dust’[shafer’s sign]
Retinal breaks
Mild iritis](https://image.slidesharecdn.com/rhegmatogenousretinaldetachment-131220122113-phpapp02/85/Rhegmatogenous-retinal-detachment-11-320.jpg)