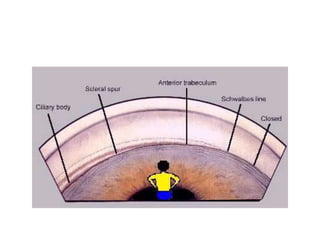
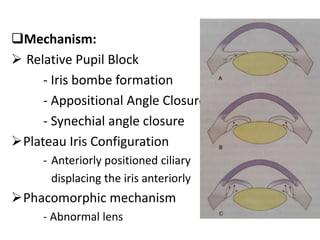
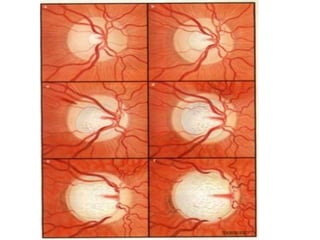
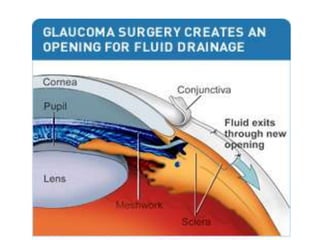
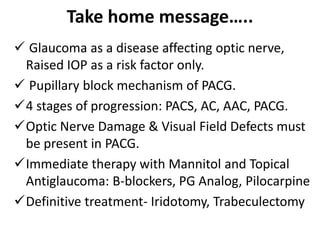
Primary angle closure glaucoma is caused by blockage of the aqueous humor outflow due to closure or narrowing of the anterior chamber angle. It progresses through stages from primary angle closure suspect to acute angle closure to angle closure glaucoma, where glaucomatous optic nerve damage and visual field defects are present. Risk factors include hyperopia, smaller anterior chamber angle, older age, and Asian ethnicity. Treatment begins with intravenous mannitol or glycerol to lower pressure urgently, followed by topical eye drop medications like beta-blockers or pilocarpine. The definitive treatment is laser iridotomy or trabeculectomy surgery to permanently open the drainage angle.