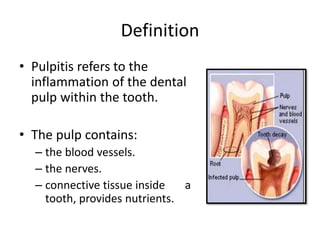
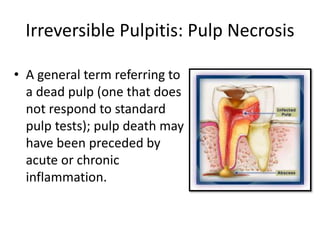
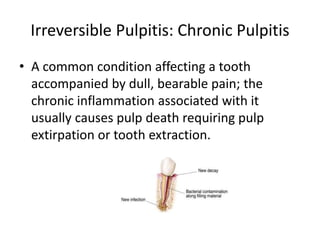
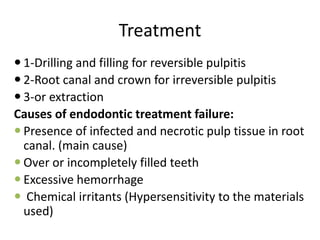
Pulpitis refers to inflammation of the dental pulp within a tooth. It is usually caused by bacterial infection from dental caries, tooth fractures, chemical or thermal irritants, or traumatic exposure. There are two main types - reversible pulpitis, which causes temporary pain that resolves on its own, and irreversible pulpitis, which leads to permanent pulp necrosis if left untreated. Symptoms include tooth pain exacerbated by hot or cold that may become constant in irreversible pulpitis. Histopathological examination shows varying degrees of inflammatory cell infiltration and destruction depending on the severity and duration of the insult. Treatment involves root canals or extractions to remove non-vital pulp tissue.