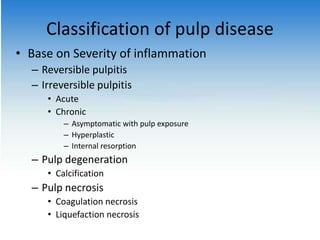
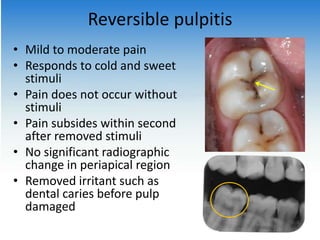
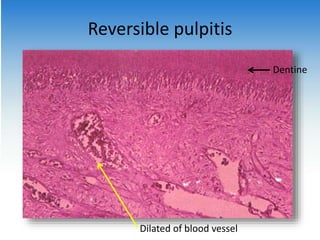
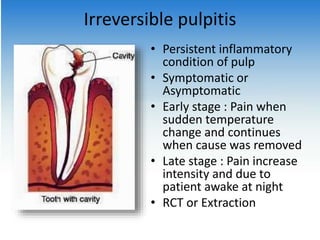
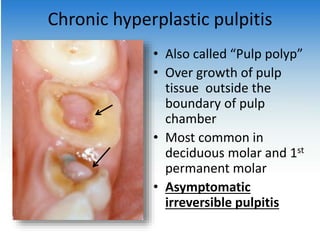
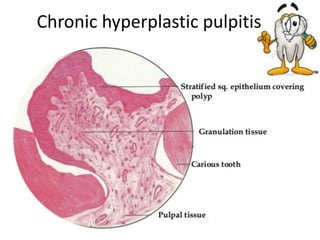
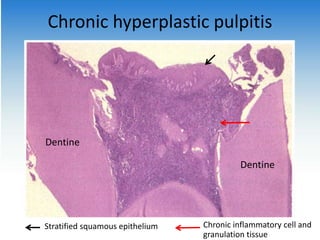
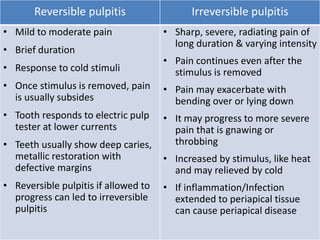
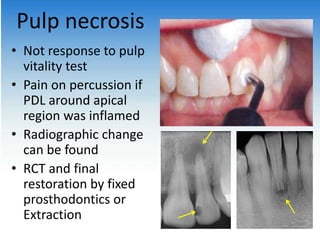
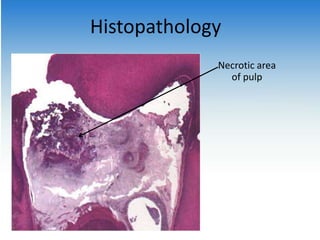
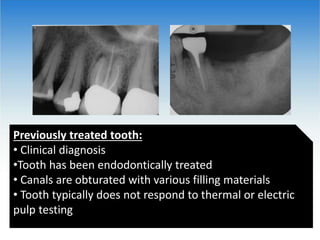
This document discusses disease of the pulp, including classification and types. It describes reversible and irreversible pulpitis, with reversible pulpitis causing mild to moderate pain in response to stimuli that subsides after removal of the stimuli. Irreversible pulpitis causes persistent pain even after stimulus removal and can progress to pulp necrosis with total or partial death of the pulp. Other conditions discussed include chronic hyperplastic pulpitis, previously treated teeth, and teeth with previously initiated therapy.