Embed presentation
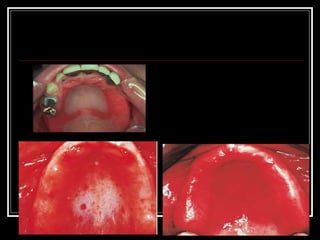
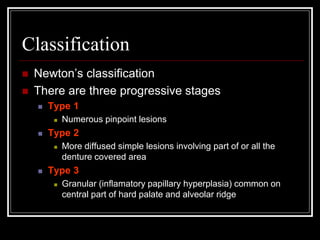
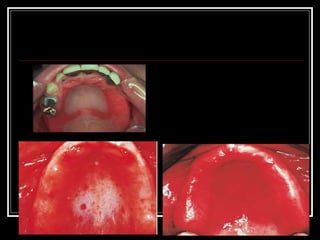
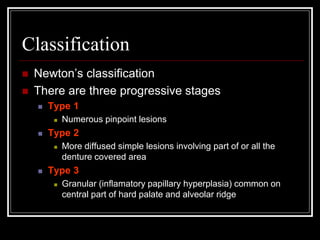
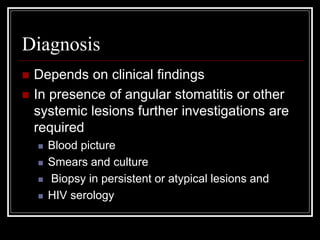
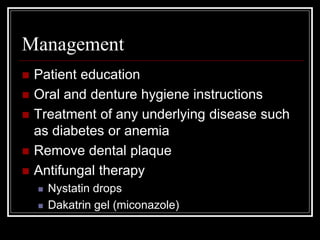
Denture Induced Stomatitis, also known as denture sore mouth, is a common condition affecting up to 70% of denture wearers, characterized by erythema and swelling of the palate mucosa in contact with the dentures. It is caused mainly by Candida albicans accumulating on dentures due to poor oral and denture hygiene. Treatment involves improving hygiene, removing dental plaque from dentures and mucosa, and using antifungal medications like nystatin drops or miconazole gel.