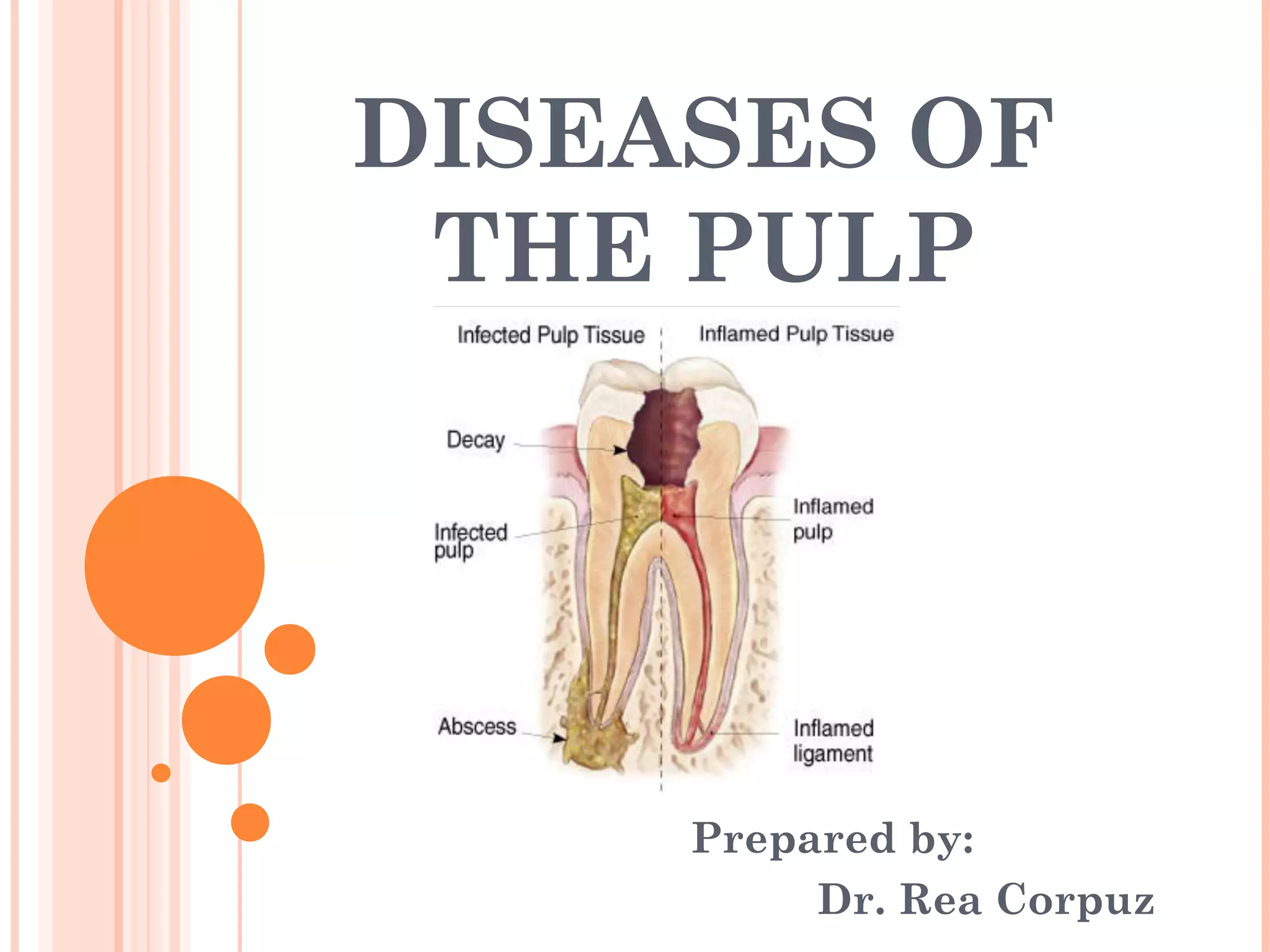
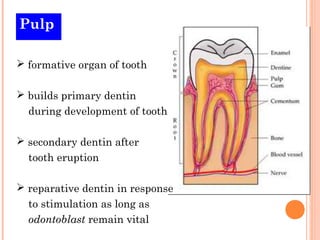
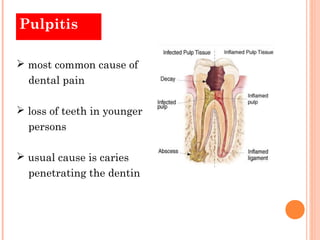
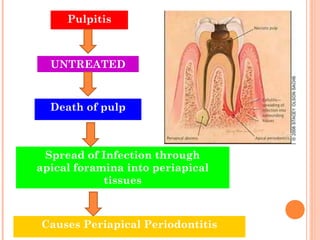
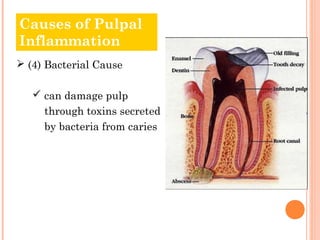
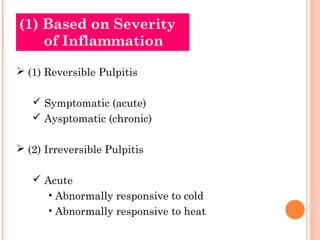
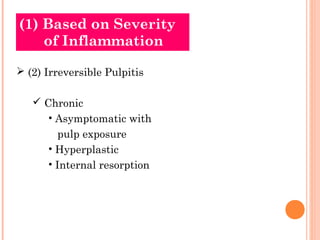
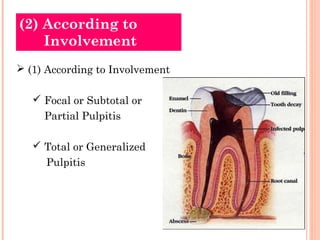
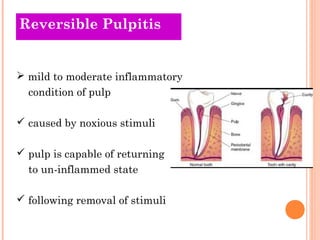
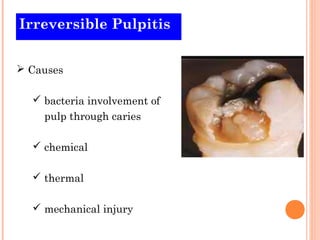
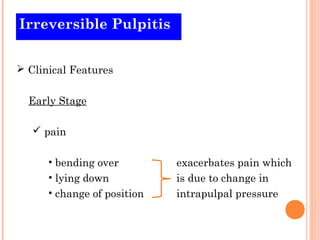
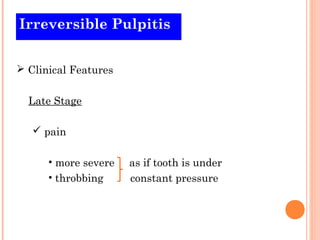
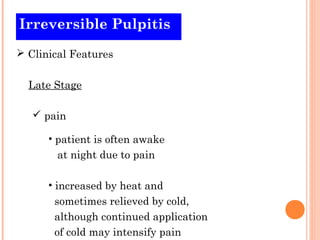
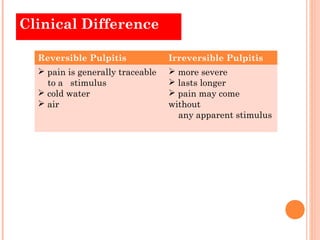
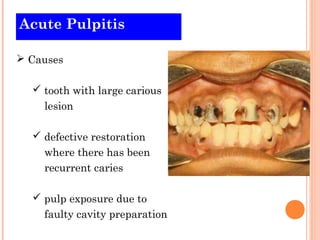
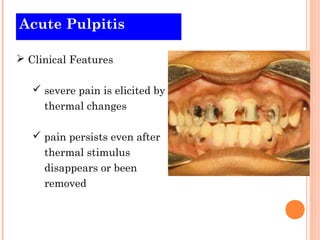
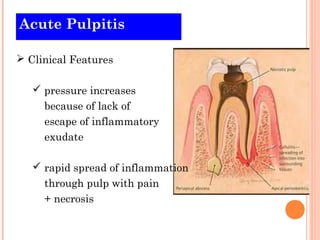
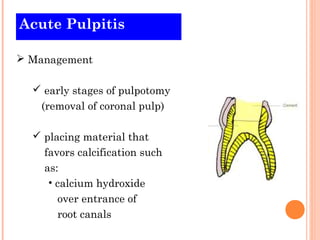
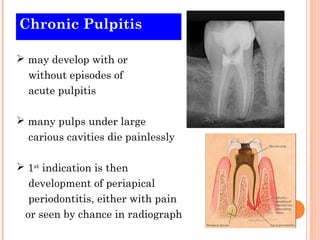
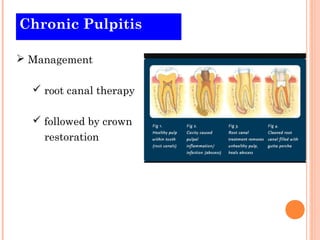
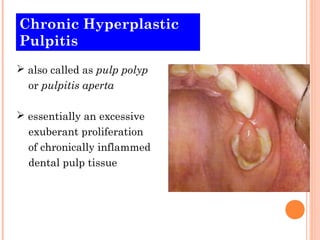
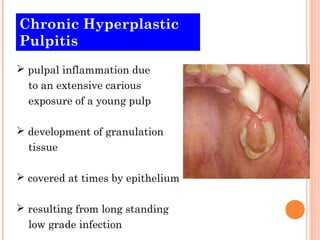
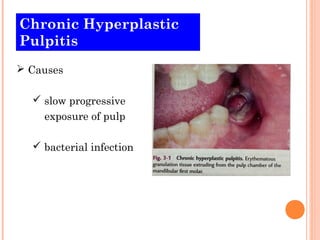
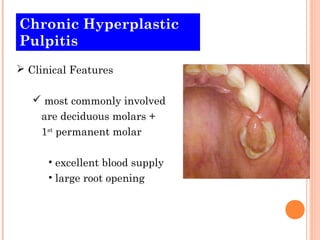
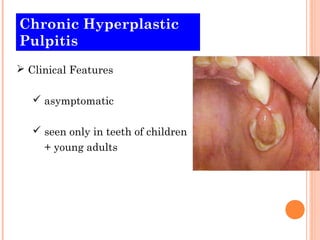
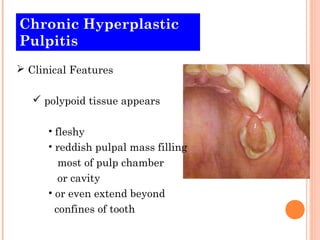
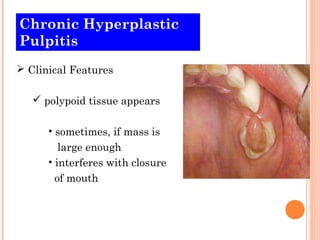
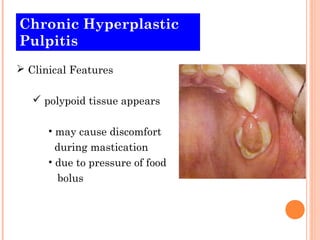
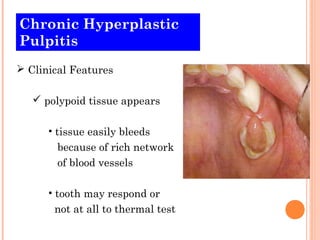
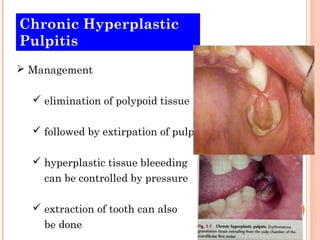
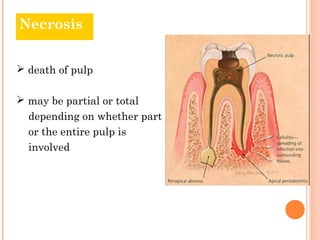
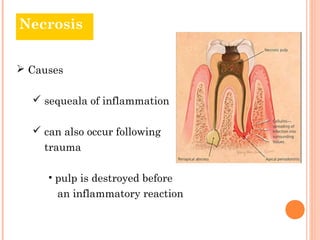
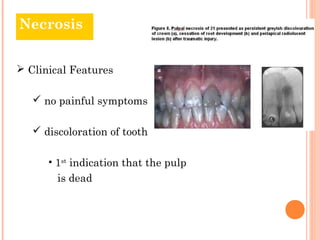
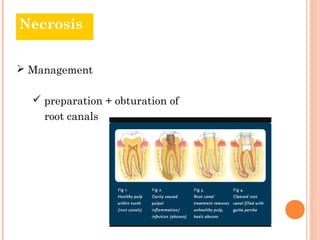
The document discusses diseases of the dental pulp, including pulpitis and necrosis. It defines the pulp as the formative organ of the tooth that builds dentin. Pulpitis is the most common cause of dental pain and can be reversible or irreversible depending on the severity of inflammation. Untreated pulpitis can lead to necrosis or death of the pulp. Causes include mechanical, thermal, chemical, and bacterial factors. Management involves removal of irritants and root canal treatment if needed.