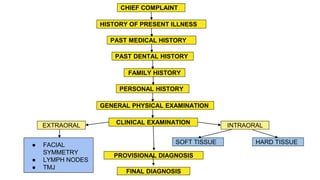
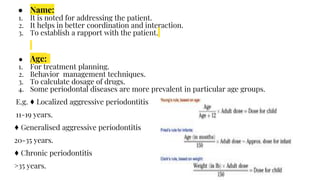
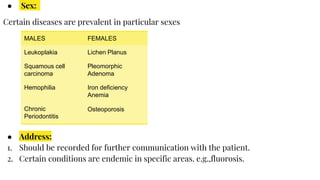
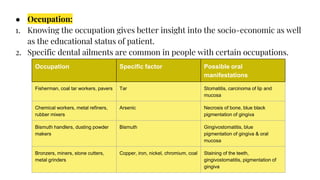
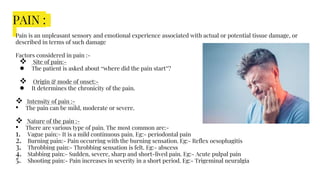
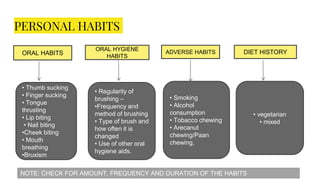
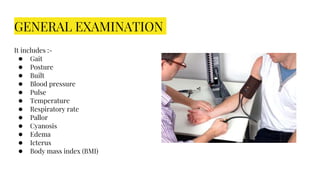
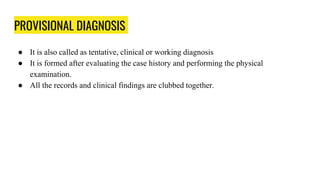
The document provides details about taking a thorough case history for periodontal patients. It emphasizes that case history recording is the first and most important step, as it allows for correct diagnosis and treatment planning. The case history should include chief complaint, history of present illness, past medical/dental history, family history, personal habits, general examination, and intraoral and extraoral examinations. Taking a comprehensive case history provides important insights into the patient's condition and relevant social, medical, and dental factors.