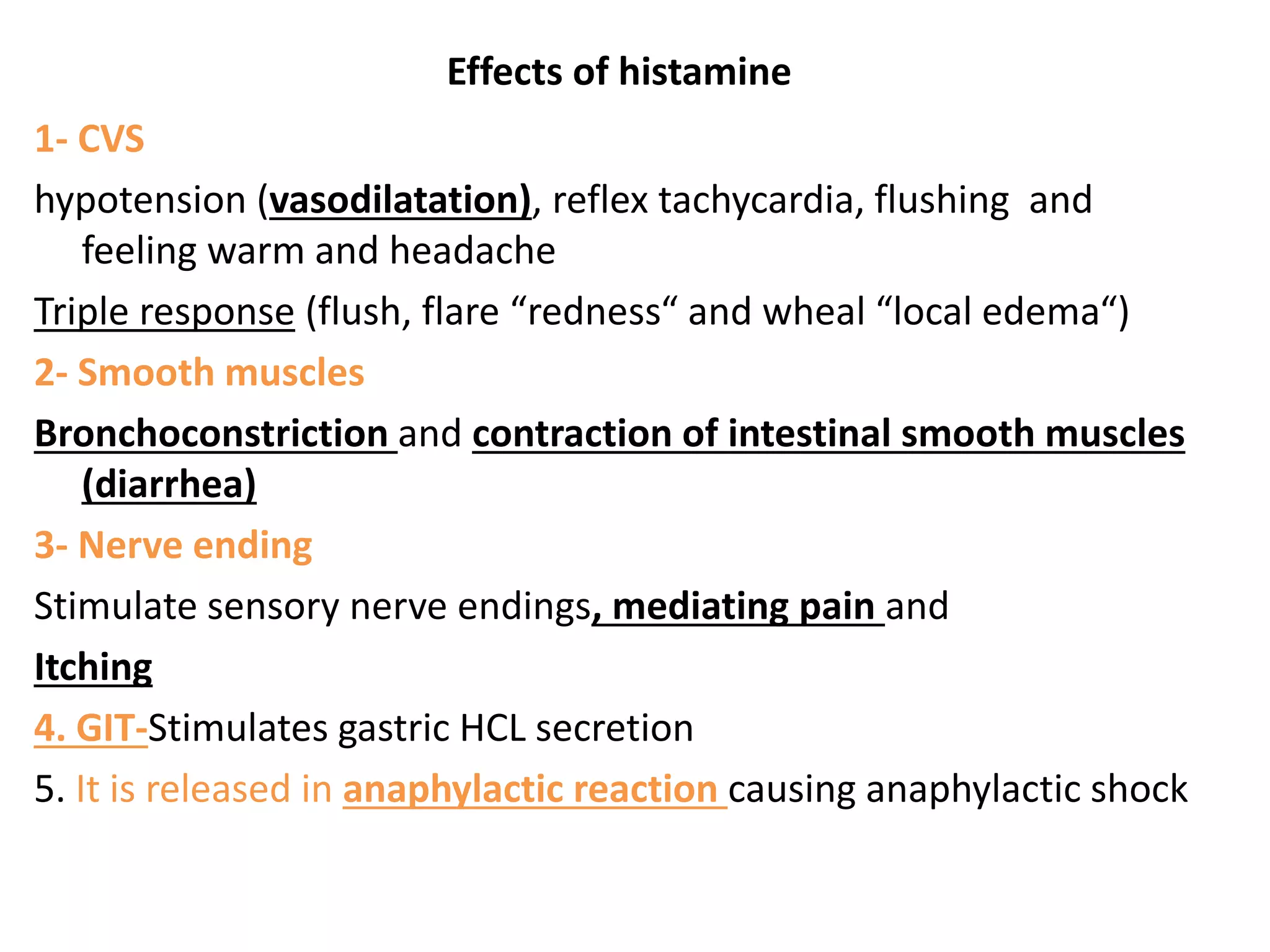
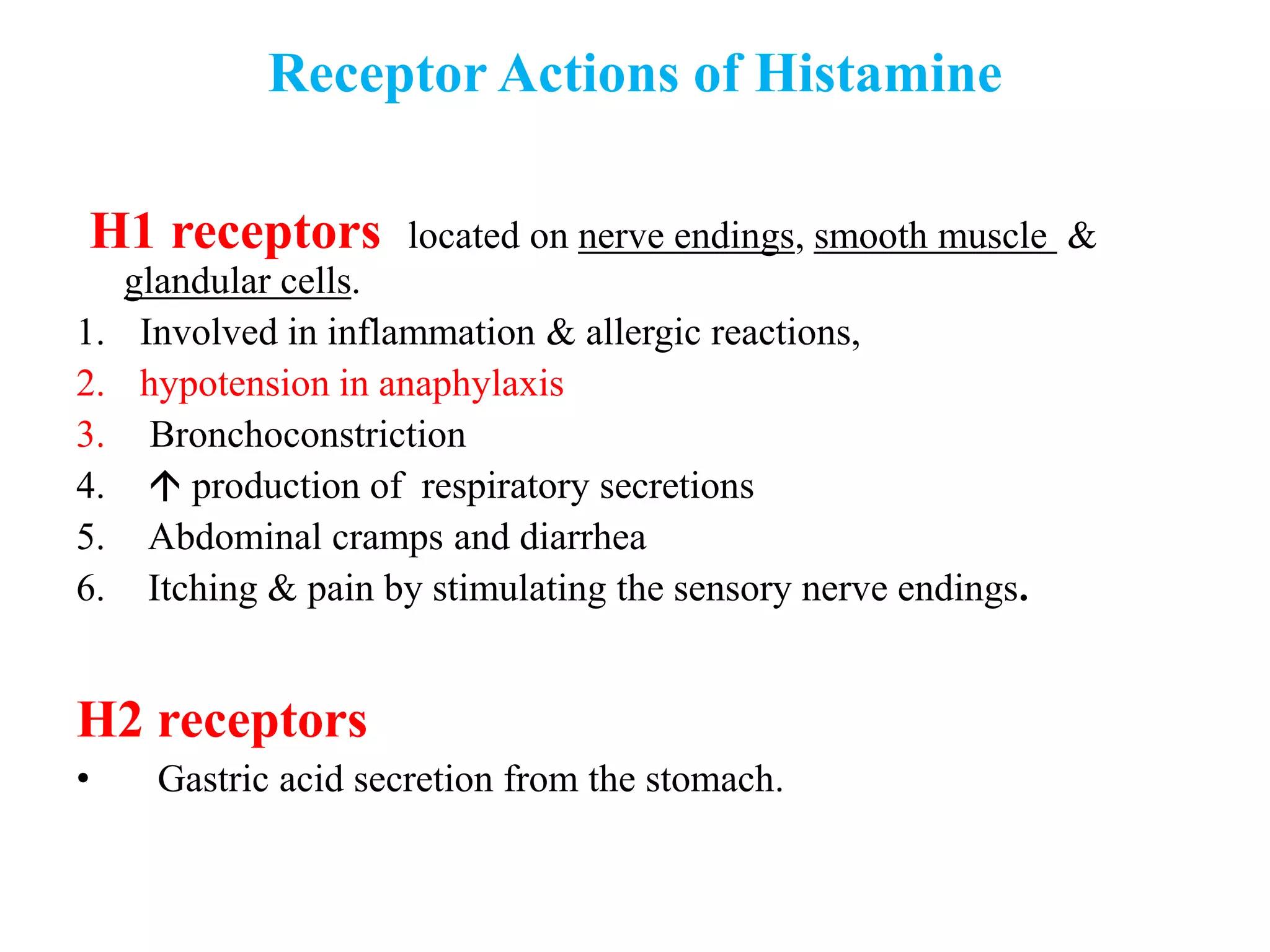
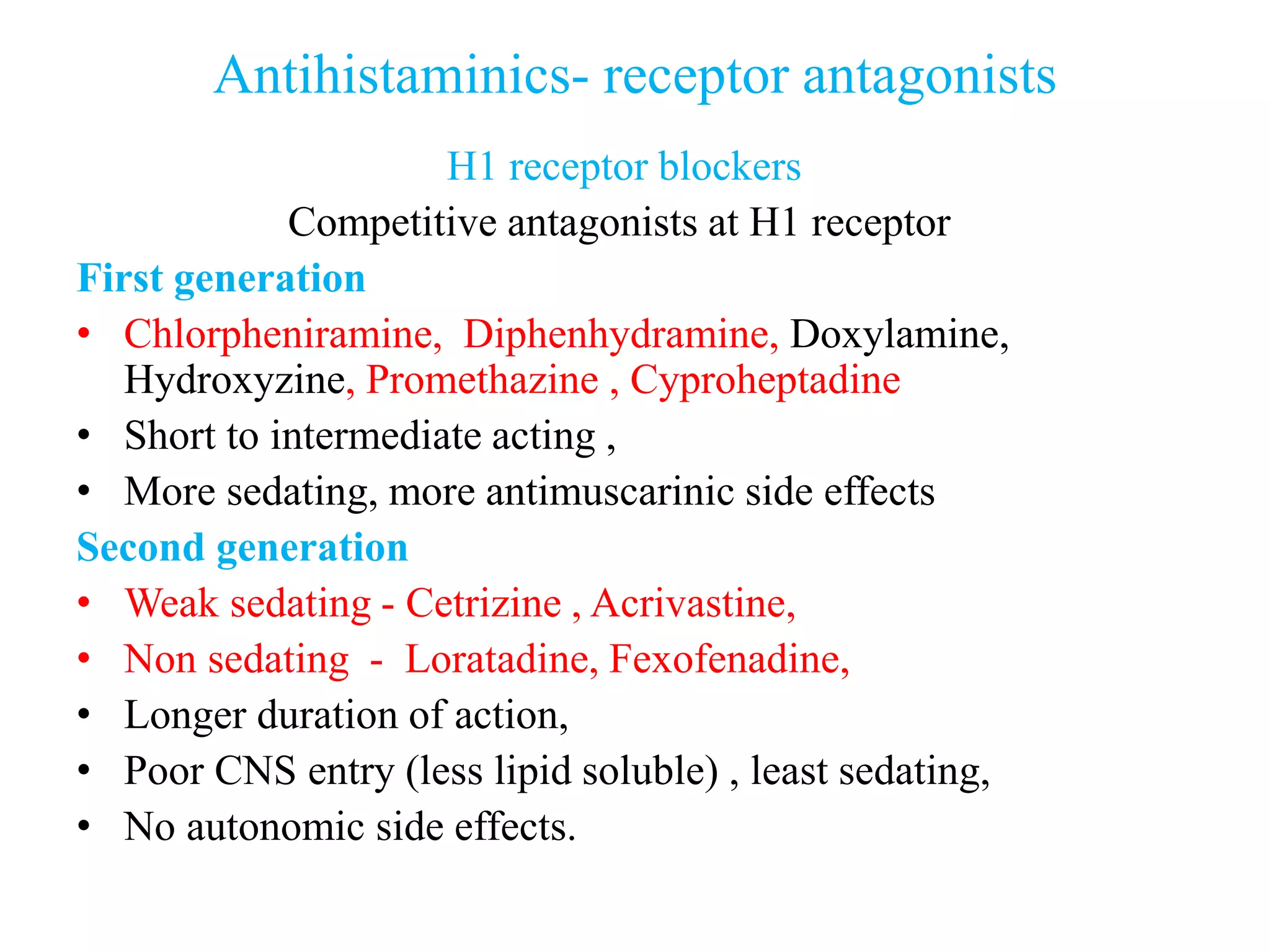
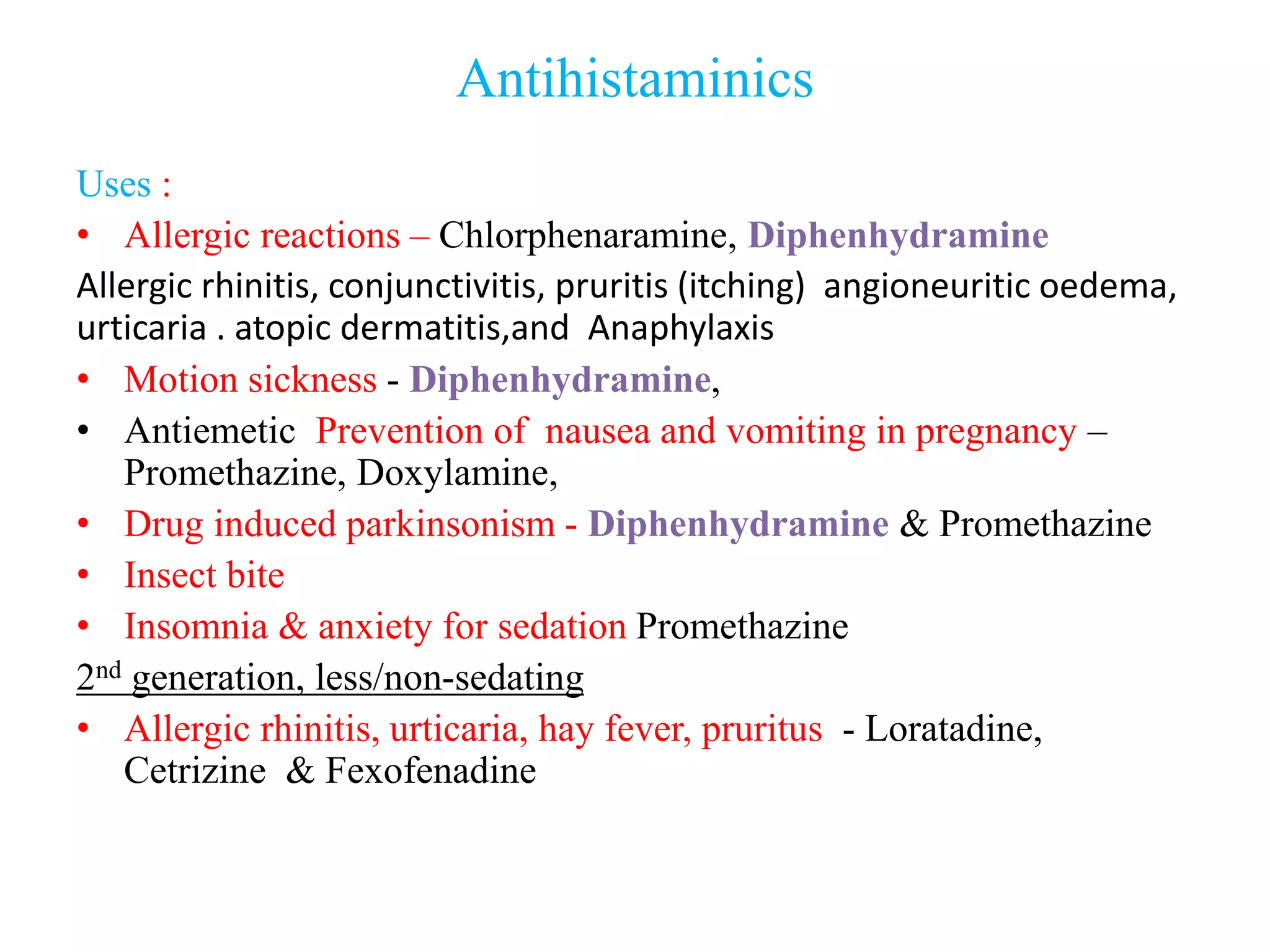
Histamine is a biologically active amine released from mast cells and basophils in response to allergens and other stimuli, causing allergic reactions and lowering blood pressure. It binds to H1 and H2 receptors. H1 receptors mediate allergic symptoms, lowering blood pressure, bronchoconstriction, and gastric acid secretion. Antihistamines like chlorpheniramine and loratadine block H1 receptors, treating allergies, motion sickness, and insomnia with varying side effects. H2 receptor blockers like cimetidine and ranitidine inhibit gastric acid secretion, treating ulcers and reflux. Second generation antihistamines have fewer anticholinergic and sedative side