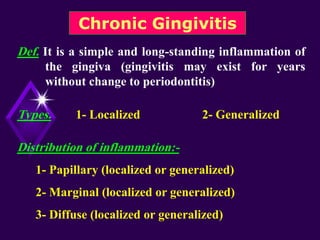
Clinical features of gingivitis include:
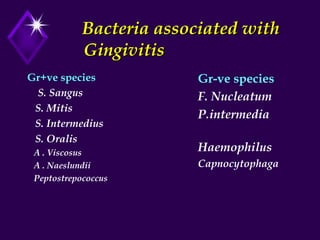
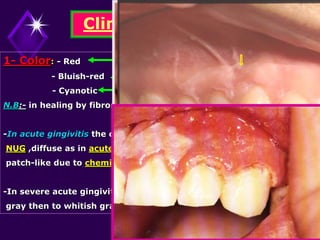
1. The gingiva appears red, swollen, and bleeds easily when probed due to inflammatory cell infiltration and increased vascularity.
2. Interdental papillae become blunted and bulbous as they bulge out between teeth.
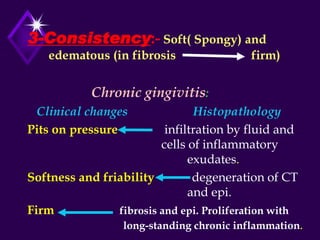
3. Histopathology shows inflammatory cell infiltration, ulceration of sulcular epithelium, edema, and fibrosis in long-standing cases.
Treatment involves thorough scaling, removing local irritants, improving plaque control, and oral hygiene instruction. The prognosis is generally excellent.