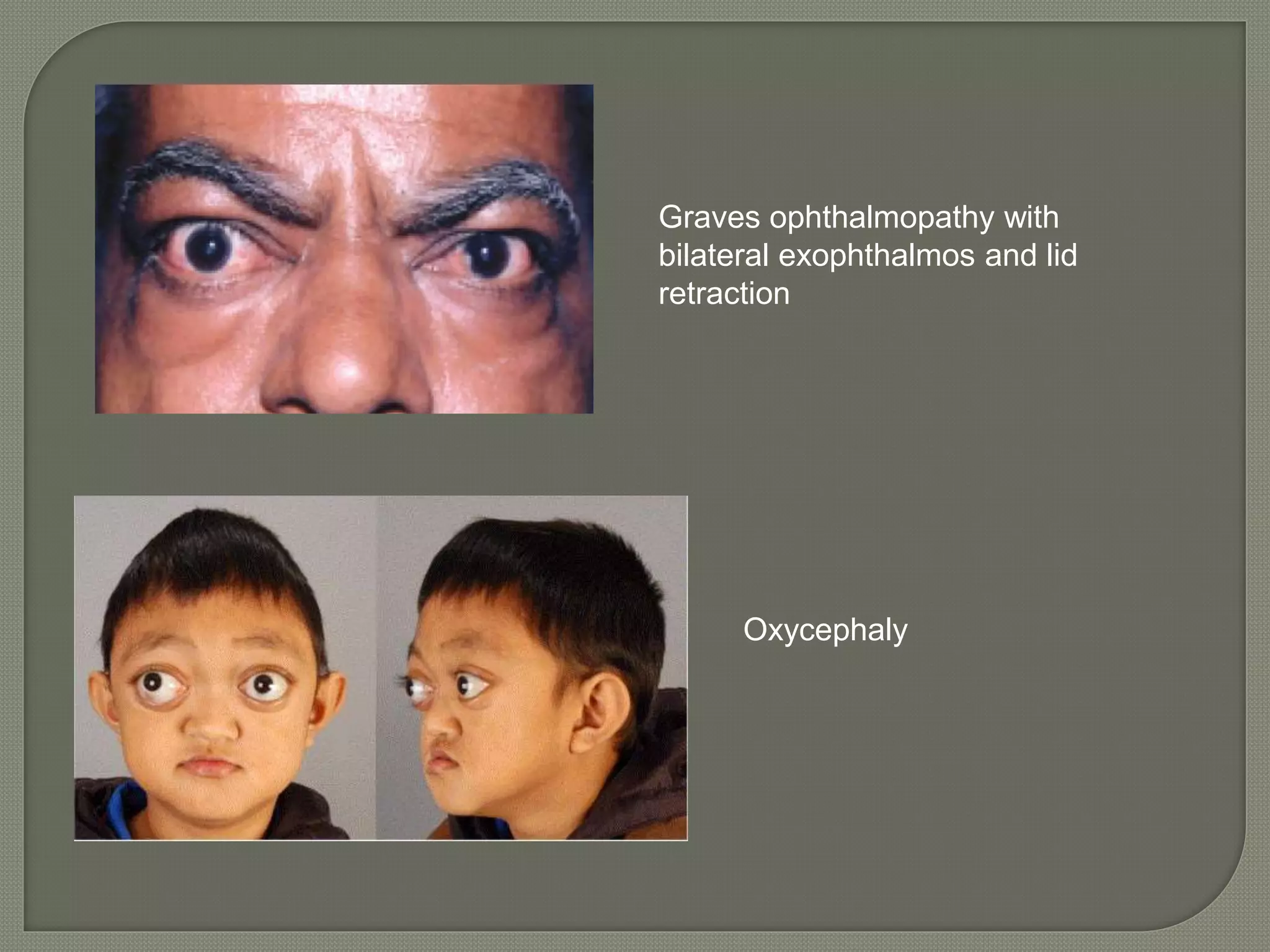
This document discusses proptosis (forward displacement of the eyeball), its causes, signs, symptoms, and evaluation. Proptosis can be unilateral or bilateral, acute or intermittent. It may be caused by congenital defects, trauma, infections, vascular lesions, cysts, tumors, or endocrine disorders like Graves' disease. Evaluation involves inspection, palpation, tests of eye movement and vision, exophthalmometry to measure protrusion, and diagnostic imaging or biopsy when indicated based on suspected etiology.