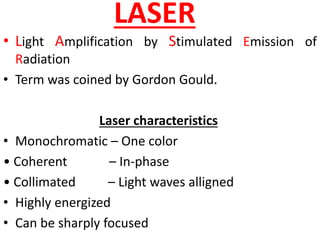
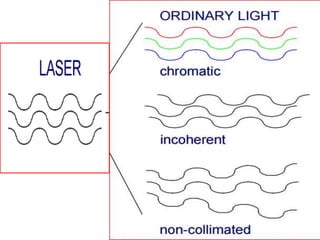
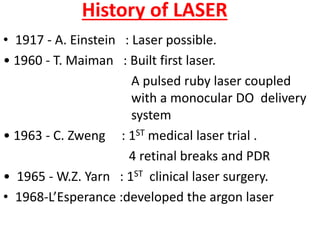
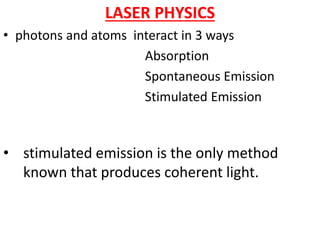
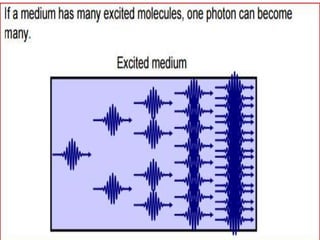
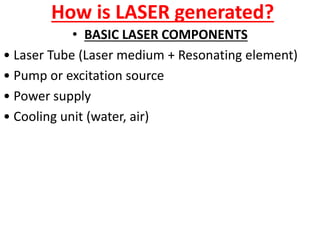
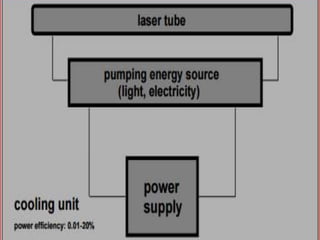
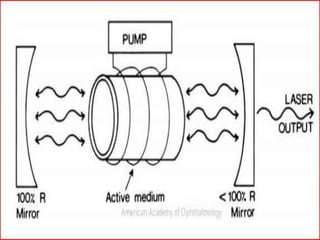
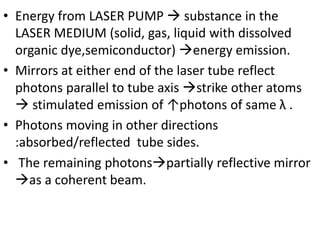
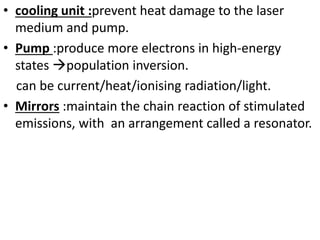
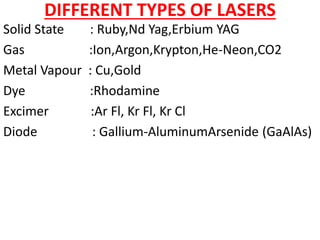
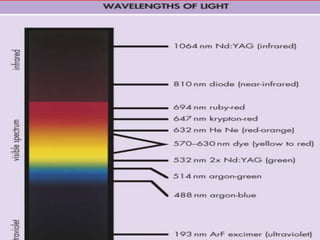
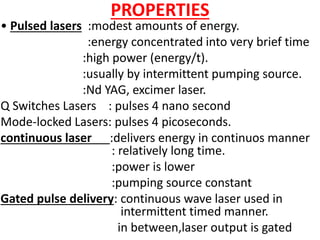
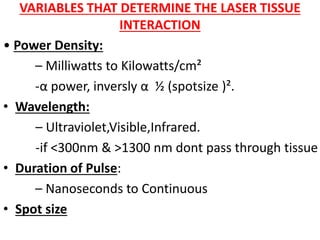
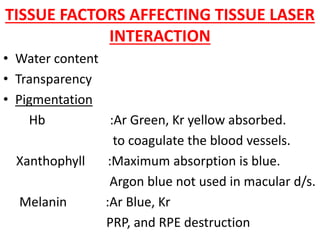
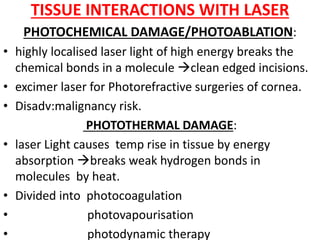
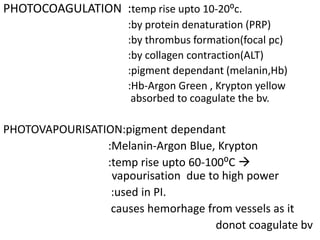
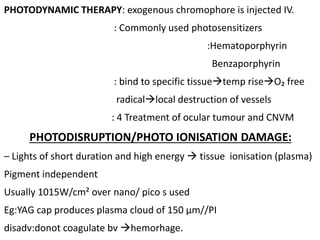
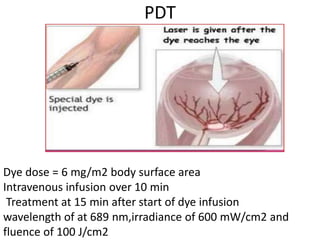
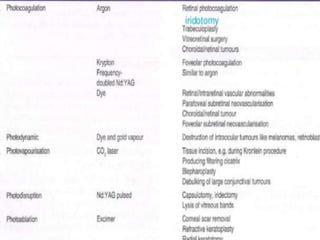
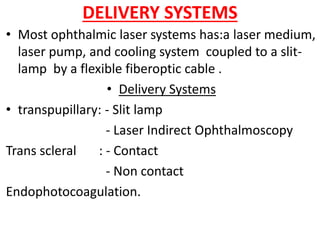
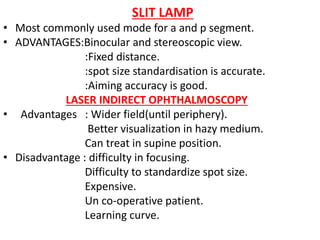
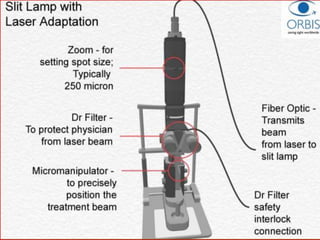
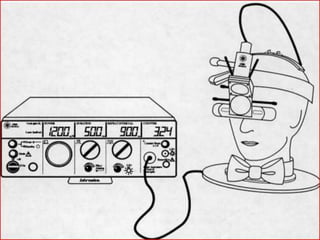
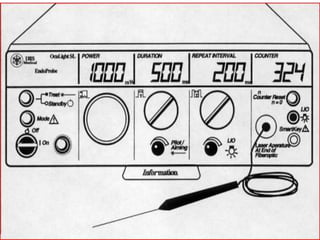
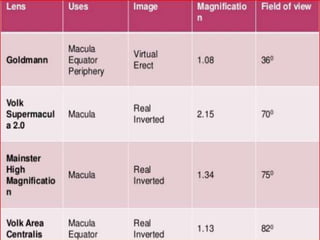
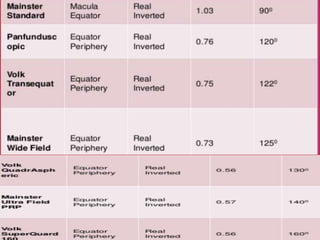
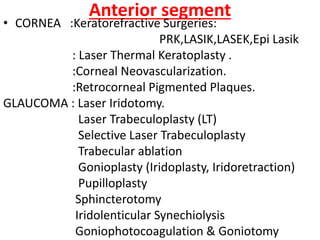
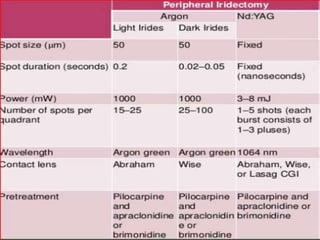
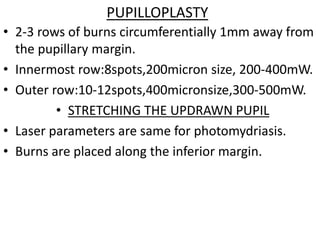
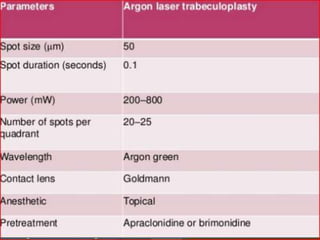
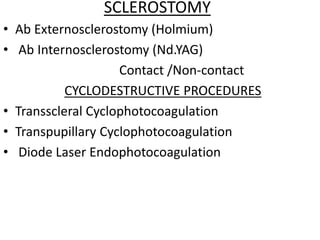
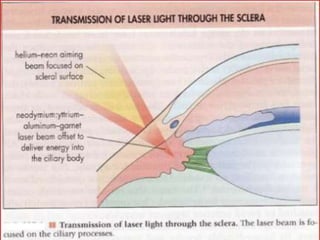
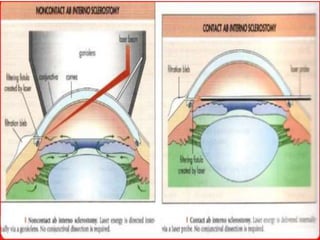
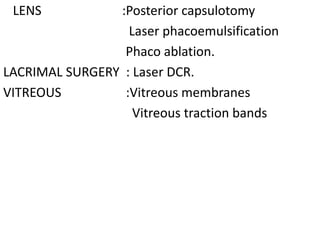
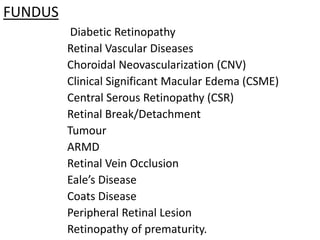
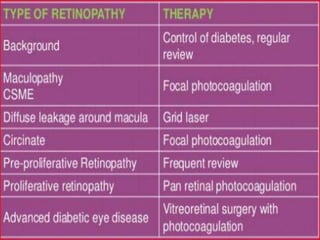
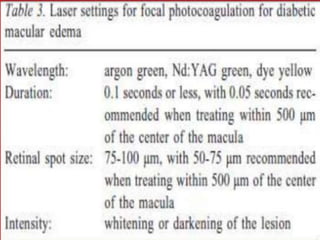
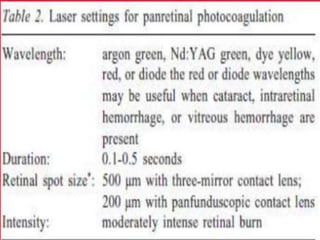
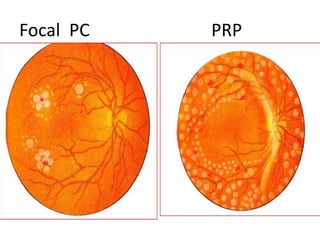
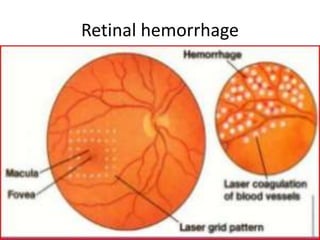
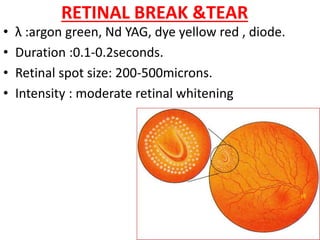
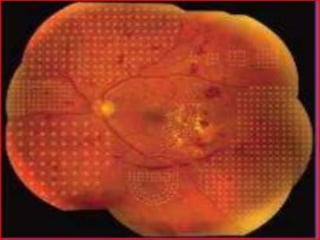
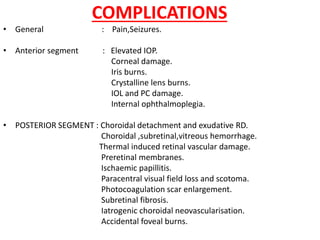
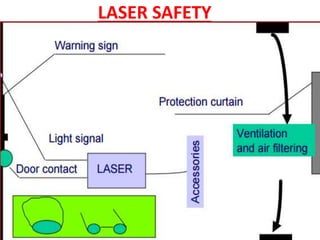
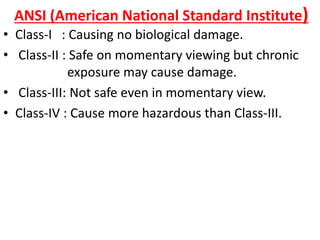
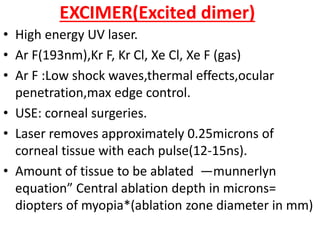
This document provides an overview of lasers used in ophthalmology. It discusses the history and physics of lasers, describing key laser characteristics and components. Different types of lasers are outlined, along with factors that determine laser tissue interaction and complications. Applications of lasers in anterior and posterior segment eye diseases are summarized. Delivery systems including slit lamps and scanning laser ophthalmoscopes are also covered, along with safety considerations.