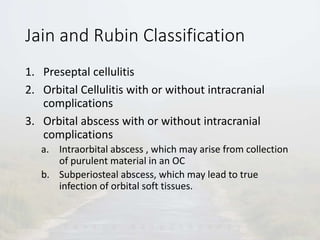
Orbital cellulitis is an inflammatory condition affecting the tissues behind the orbital septum. It typically presents with eyelid swelling and redness, vision loss, and pain with eye movement. The most common causes are sinus infections or infections of nearby structures that spread. Prompt diagnosis and treatment with antibiotics and imaging such as CT are important to prevent complications like abscesses or intracranial infections. Surgical drainage may be needed for abscesses. With appropriate treatment, outcomes have improved but orbital cellulitis still poses risks if not addressed quickly.