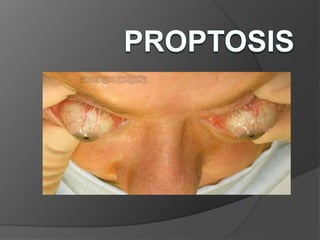
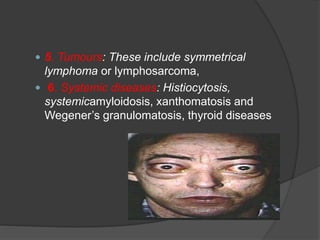
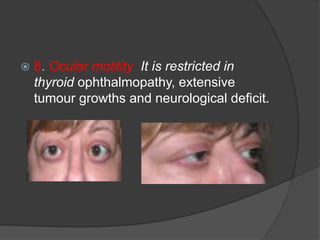
Proptosis is the forward displacement of the eyeball beyond the orbital margins. It can be unilateral, bilateral, acute, intermittent, or pulsating. Common causes include congenital conditions, trauma, inflammation, tumors, cysts, vascular lesions, thyroid disease, and skull abnormalities. Evaluation involves clinical examination, lab tests, imaging like CT/MRI, and sometimes biopsy. Treatment aims to remove the underlying cause through procedures like surgery.