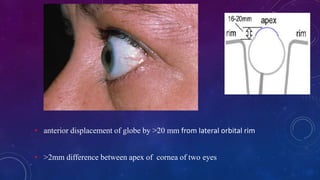
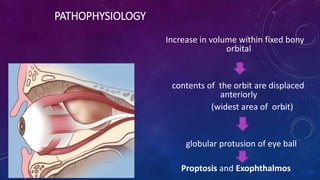
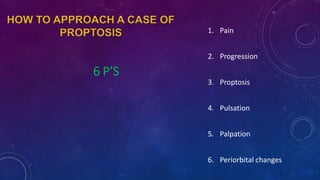
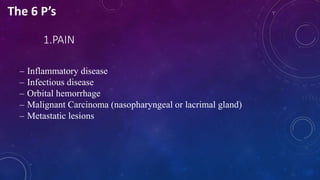
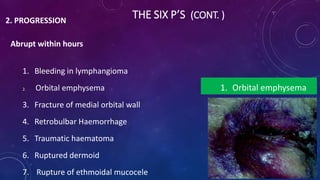
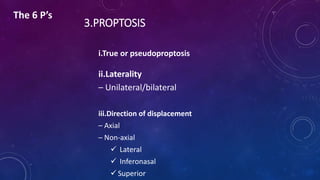
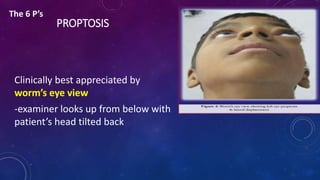
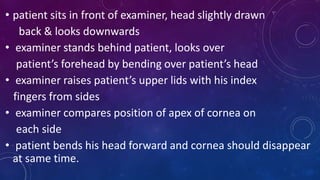
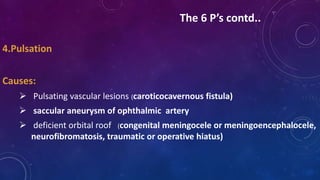
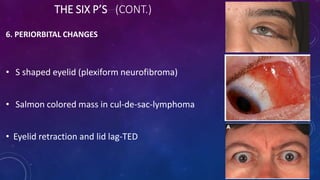
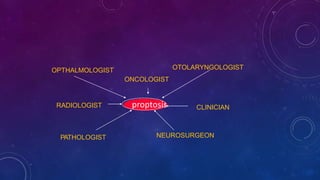
1. Proptosis is the abnormal forward displacement of the eyeball. It can be evaluated based on the 6 Ps: pain, progression, proptosis, pulsation, palpation, and periorbital changes.
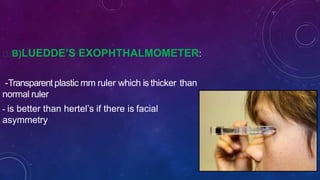
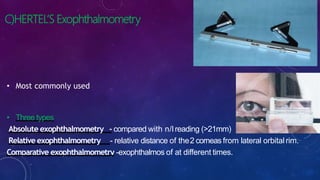
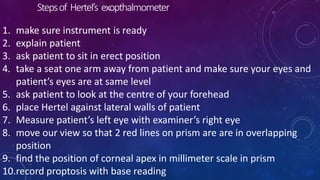
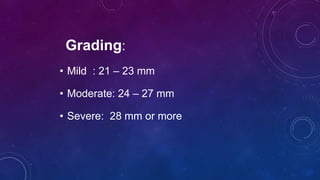
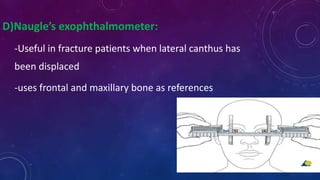
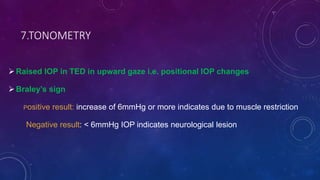
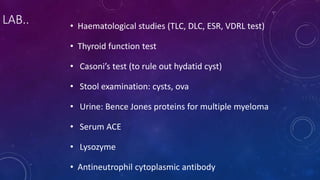
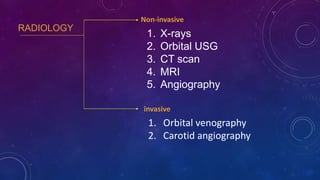
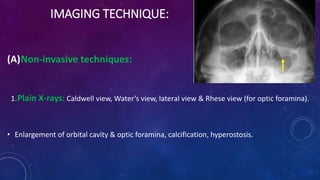
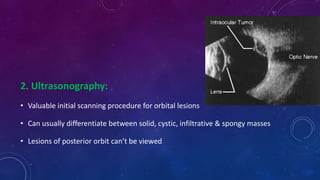
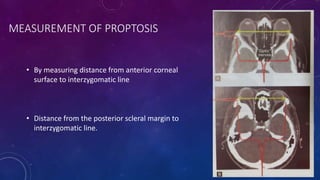
2. Clinical evaluation involves measuring the degree of proptosis using methods like Hertel's exophthalmometer. Imaging studies like CT and MRI help determine the cause and extent of proptosis.
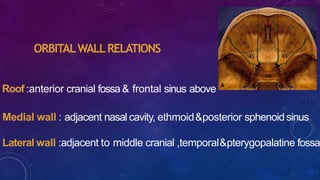
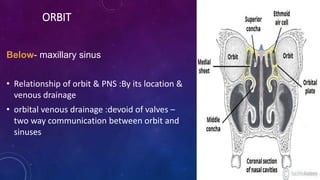
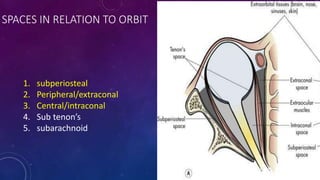
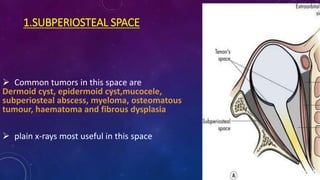
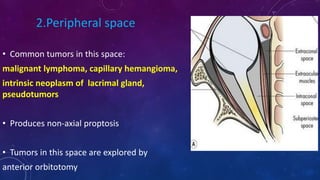
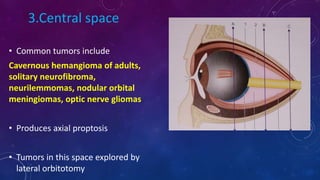
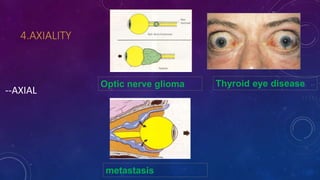
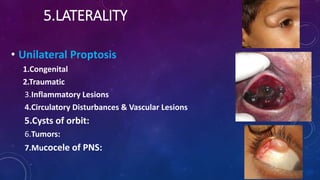
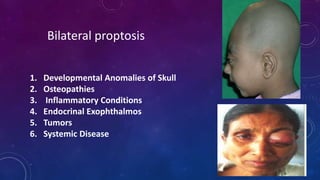
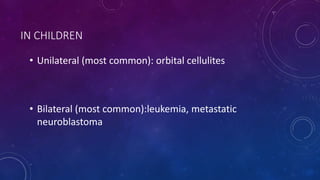
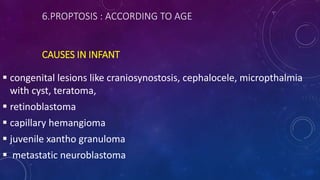
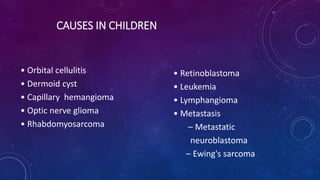
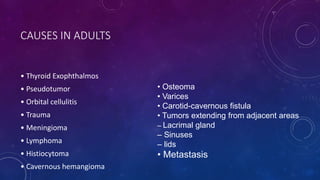
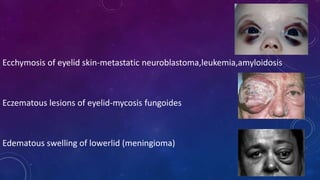
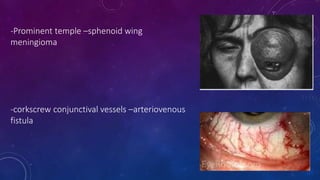
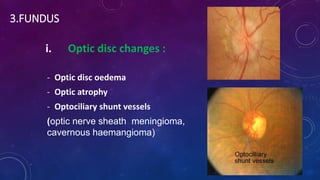
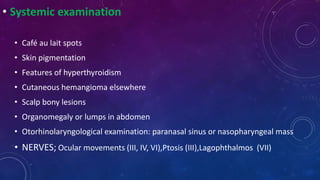
3. Common causes of proptosis include thyroid eye disease, orbital tumors, infections, vascular lesions, and trauma. The document discusses the clinical anatomy of the orbit and approaches to classify and investigate proptosis.