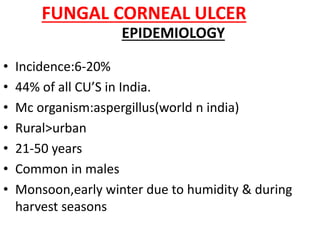
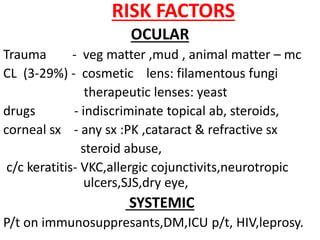
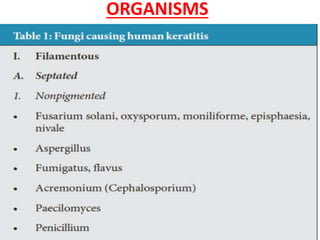
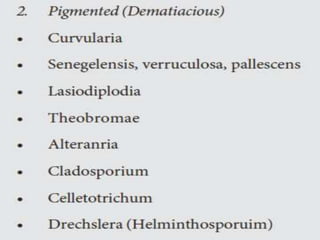
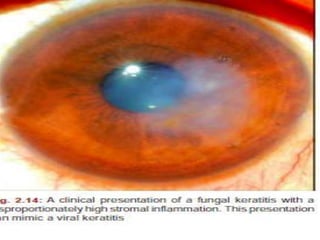
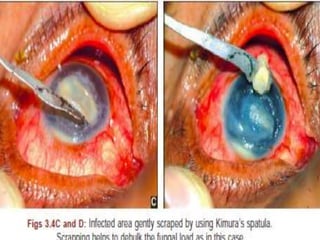
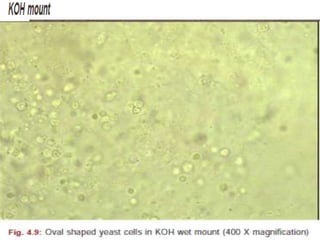
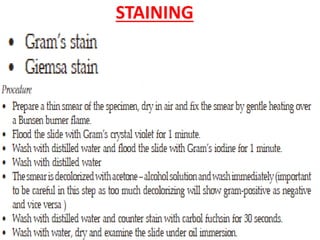
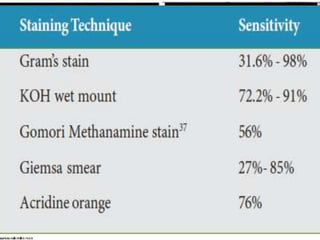
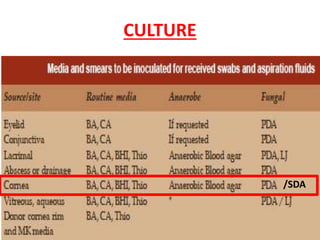
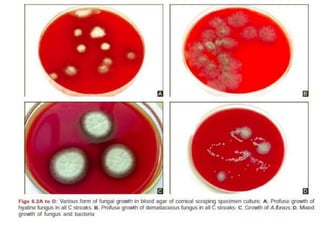
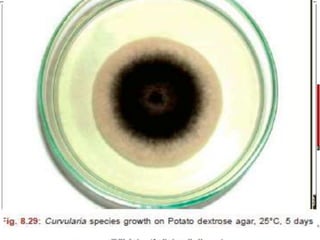
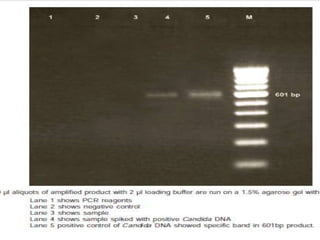
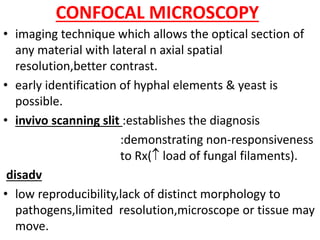
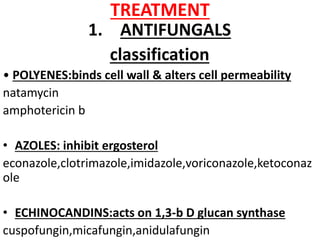
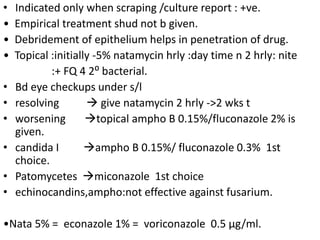
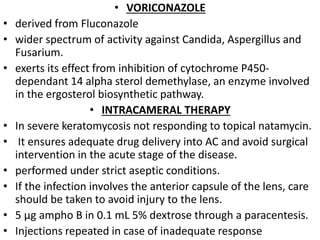
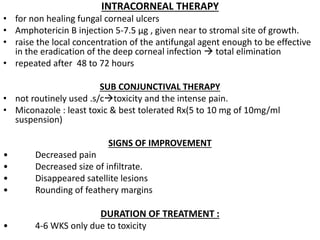
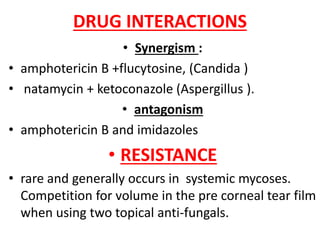
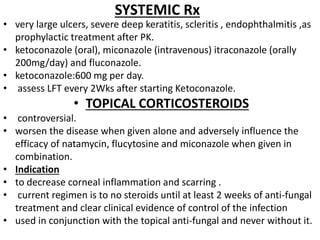
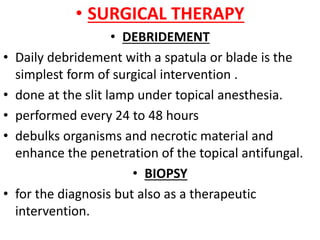
Fungal corneal ulcers are common, caused mainly by Aspergillus in India. Risk factors include ocular trauma, contact lens use, pre-existing eye conditions, and systemic immunosuppression. Diagnosis involves corneal scrapings, cultures, and stains showing fungal hyphae or spores. Treatment consists of topical natamycin or amphotericin B, sometimes with adjunctive debridement, intracameral/intracorneal injections, or therapeutic keratoplasty for severe cases. Systemic antifungals may also be used for extensive infections.