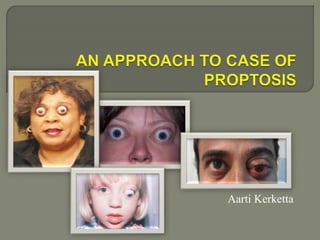
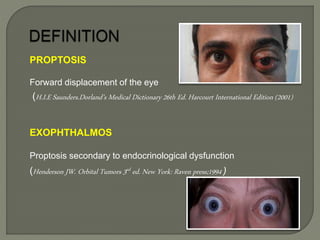
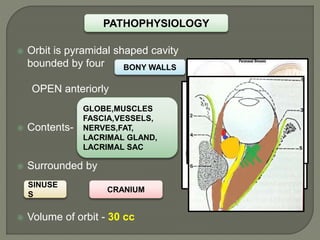
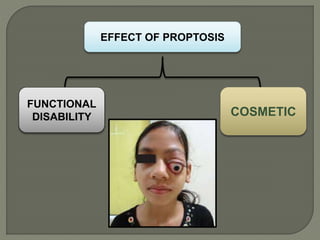
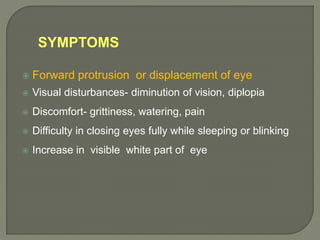
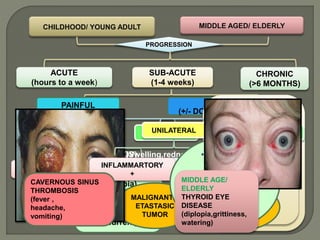
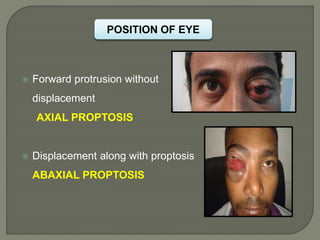
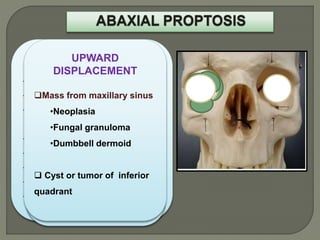
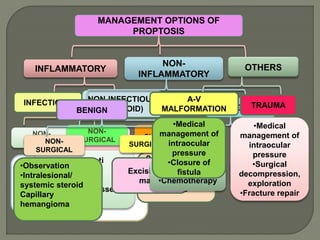
1. Proptosis refers to the forward displacement of the eye within the orbit. It can be caused by conditions affecting the orbit or endocrine system.
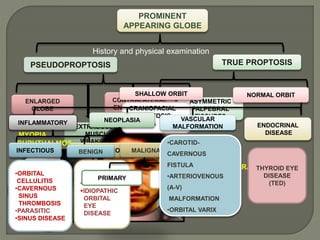
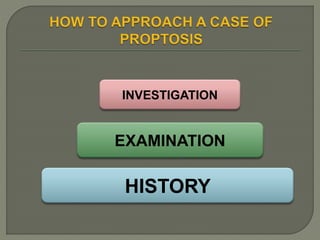
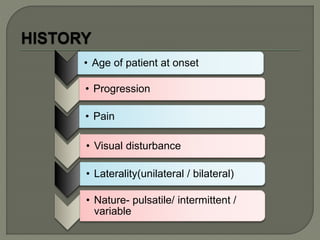
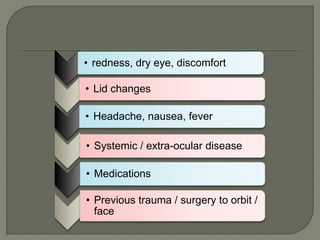
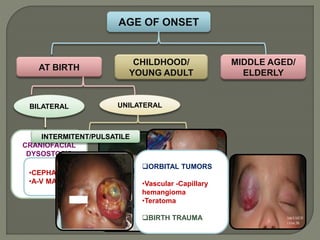
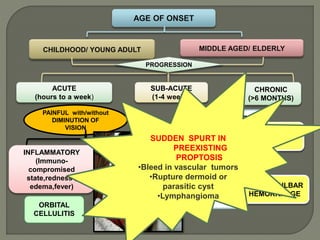
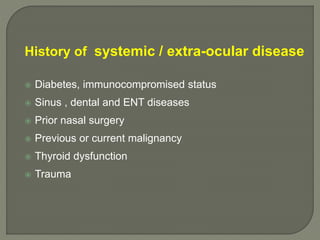
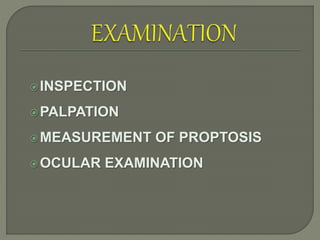
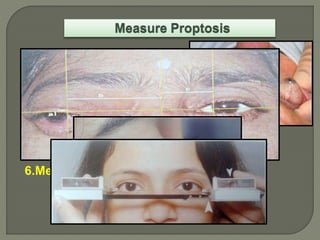
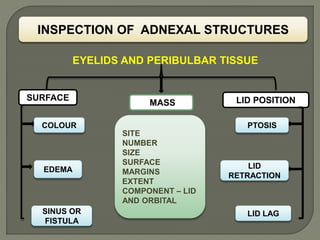
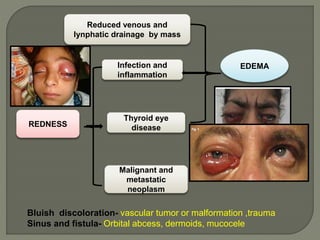
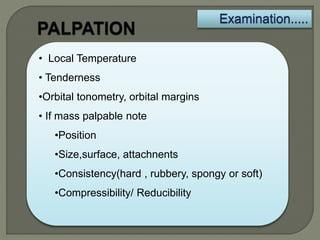
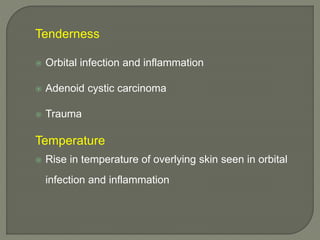
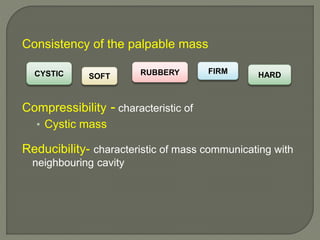
2. A thorough history and physical examination are important to determine the cause, characteristics, progression of proptosis, and assess for signs of inflammation, infection, or underlying systemic disease.
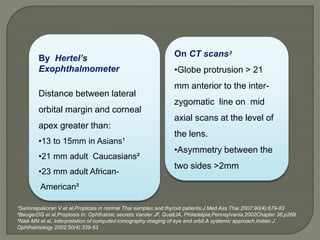
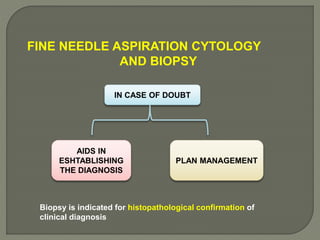
3. Imaging studies like CT and MRI help identify the location, size, and nature of any orbital lesions causing proptosis and guide management. Biopsy may be needed to confirm diagnosis in some cases.