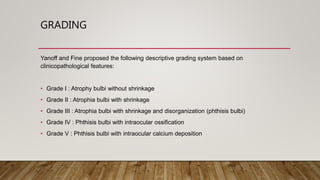
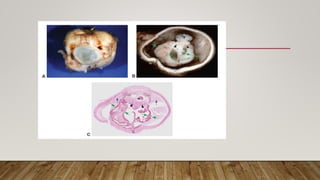
This document defines and describes phthisis bulbi, a condition where the eye shrinks and its contents become disorganized due to severe injury or disease damage. It outlines the causes of phthisis bulbi, including trauma, infection, inflammation, surgery, retinal detachment, and malignancy. A grading system is proposed based on clinical features, from atrophy without shrinkage to phthisis bulbi with intraocular ossification or calcium deposition. Signs, symptoms, pathophysiology, diagnosis, and management are discussed, with management focusing on alleviating pain and cosmetic rehabilitation rather than restoring vision.