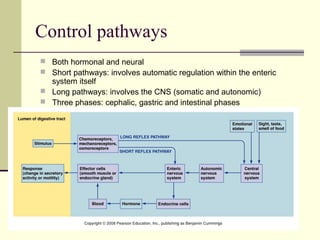
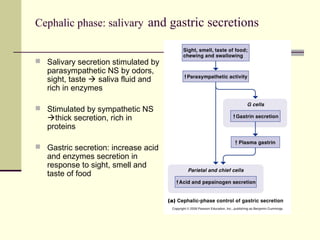
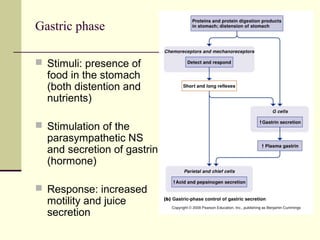
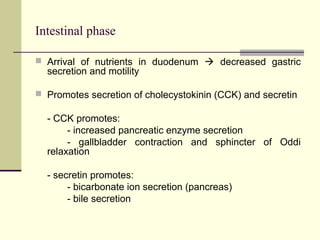
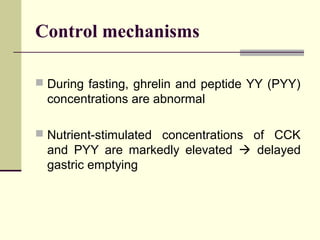
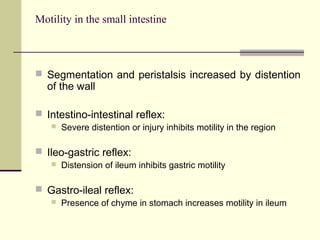
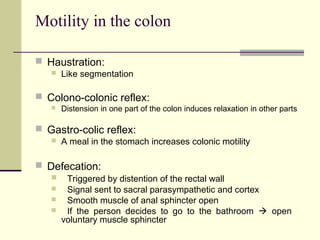
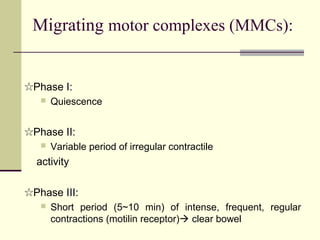
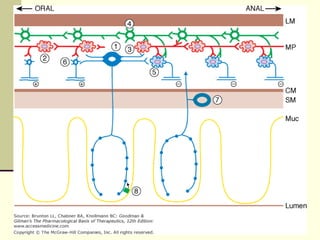
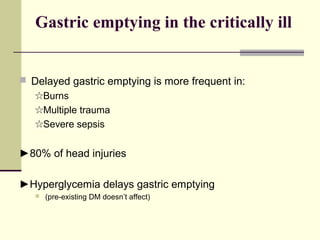
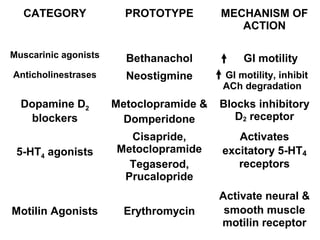
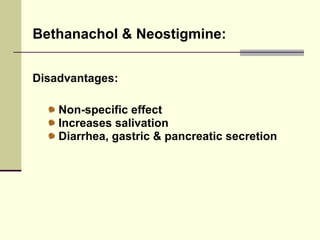
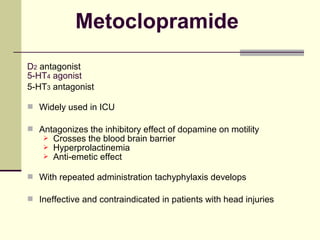
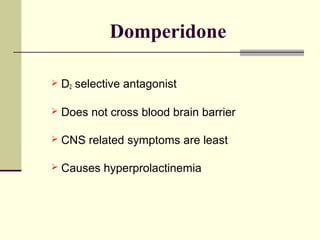
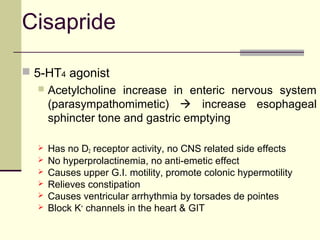
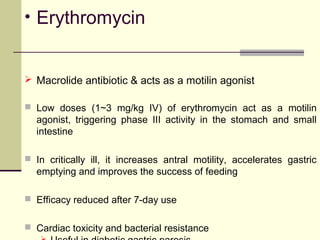
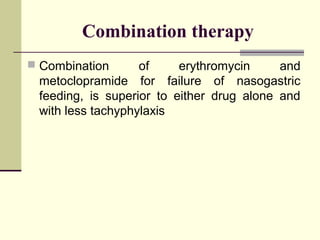
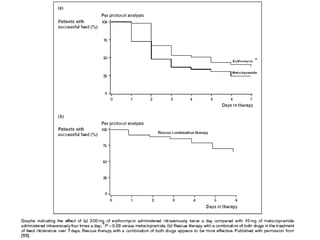
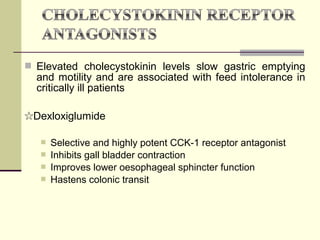
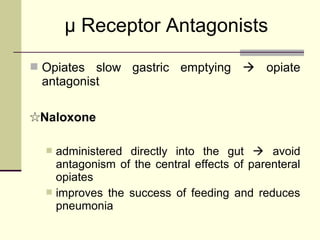
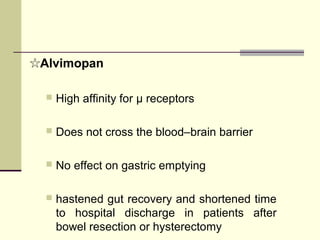
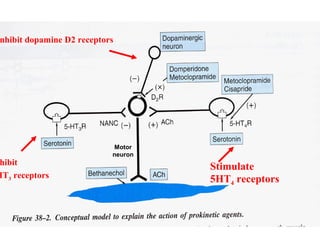
This document discusses prokinetics, which are drugs that enhance gastrointestinal motility. It describes the normal control pathways of GI motility, including hormonal and neural pathways. It then discusses various phases of GI motility including the cephalic, gastric, and intestinal phases. The document outlines several prokinetic drug categories and examples, including muscarinic agonists, anticholinesterases, dopamine D2 blockers, 5-HT4 agonists, and motilin agonists. It discusses the mechanisms of action and advantages/disadvantages of various prokinetic drugs. Novel therapies for improving GI motility in critically ill patients are also mentioned.