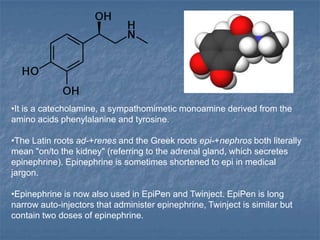
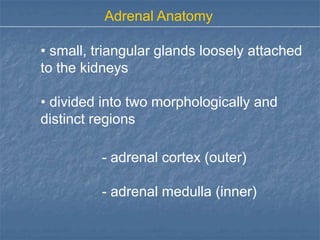
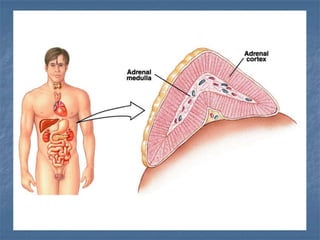
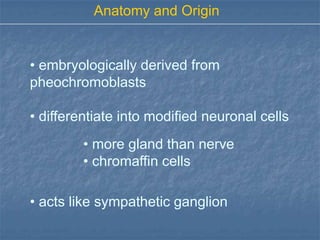
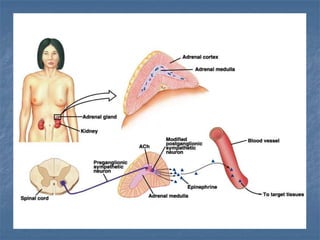
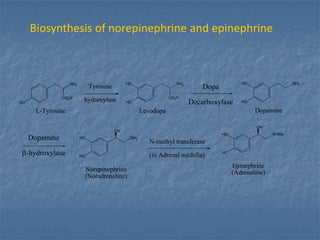
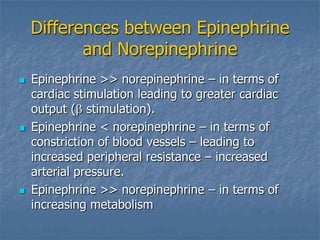
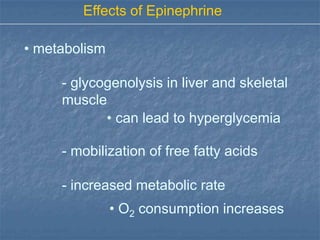
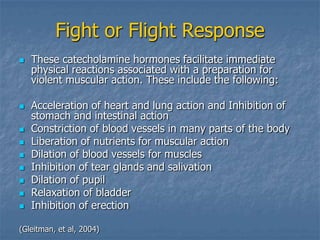
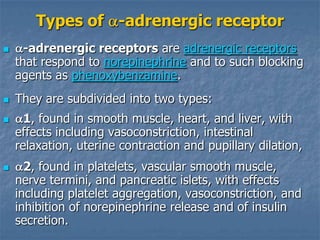
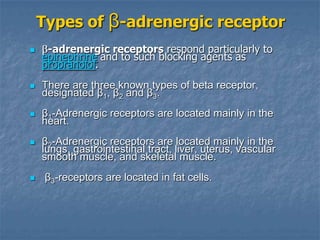
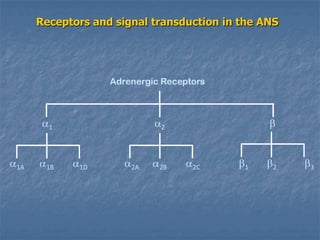
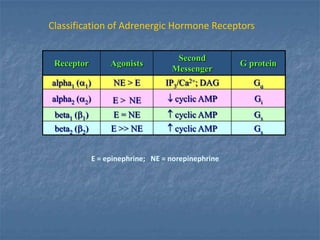
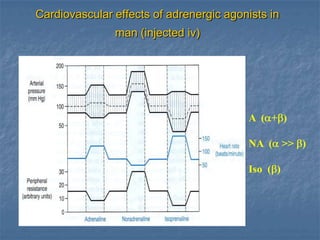
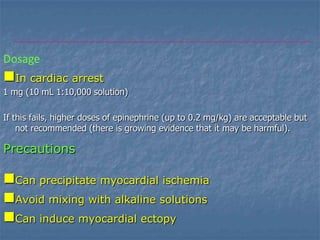
Epinephrine is a catecholamine hormone produced by the adrenal medulla. It plays an important role in the fight or flight response by increasing heart rate, redirecting blood flow, and raising blood pressure and blood glucose levels. Epinephrine is used medically to treat cardiac arrest, severe hypotension, and anaphylaxis. It is administered via injection using devices like EpiPens. Epinephrine acts on alpha and beta adrenergic receptors and stimulates the sympathetic nervous system.