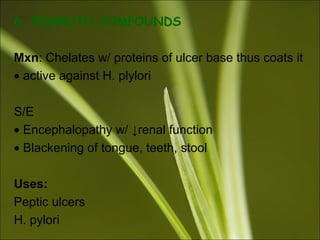
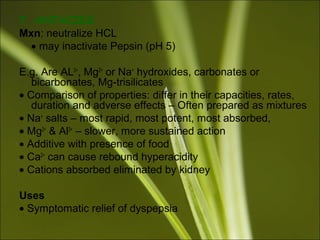
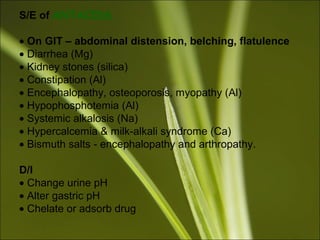
1. The document discusses drugs acting on the gastrointestinal system, focusing on drugs used to treat peptic ulcers and gastroesophageal reflux disease.
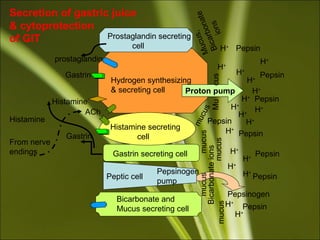
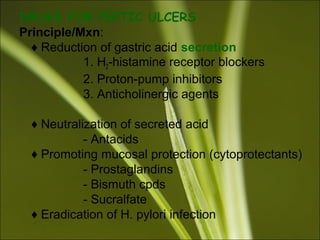
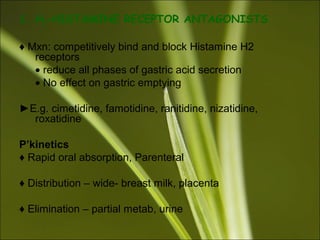
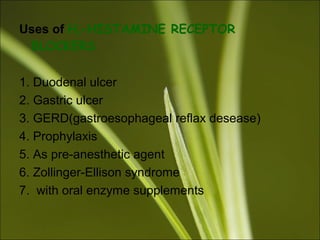
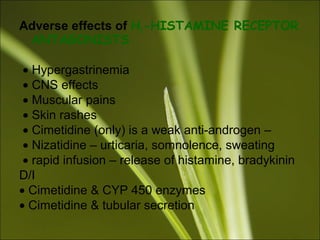
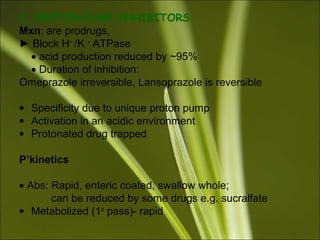
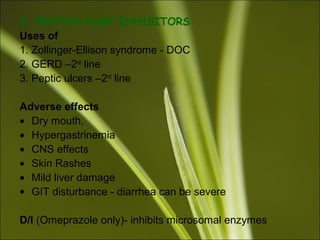
2. It describes the physiology of gastric acid secretion and the phases of stimulated secretion. Drugs that reduce acid secretion include H2 receptor blockers, proton pump inhibitors, and anticholinergic agents. Cytoprotective drugs like prostaglandins and sucralfate are also discussed.
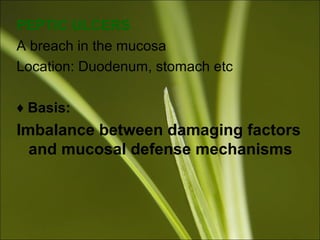
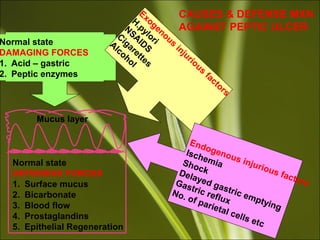
3. Causes of peptic ulcers include an imbalance between damaging factors like acid and pepsin and defensive factors like mucus and bicarbonate. Drugs covered for treating ulcers aim to reduce acid, neutralize acid, promote m


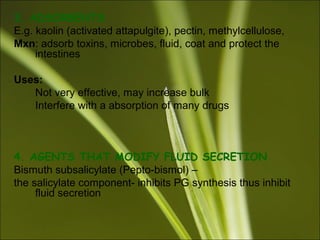
![5. SUCRALFATE (a cytoprotectant)
Mxn: form a viscous, sticky gel in the acidic environment &
coats the mucosa
• Adsorbs onto protein
P’kinetics
• Note on Administration: with food, 1hr or so with antacids
• Partial abs
S/E
Constipation –
High plasma [Al3+
] w/ ↓renal function
D/I –
Chelates some drugs ∟↓absorption e.g. phenytoin, digoxin
Uses
• Peptic ulcers – long term maintenance
• Prophylaxis – stress ulcers](https://image.slidesharecdn.com/kamurengit-150803101008-lva1-app6891/85/GIT-pharmacology-16-320.jpg)