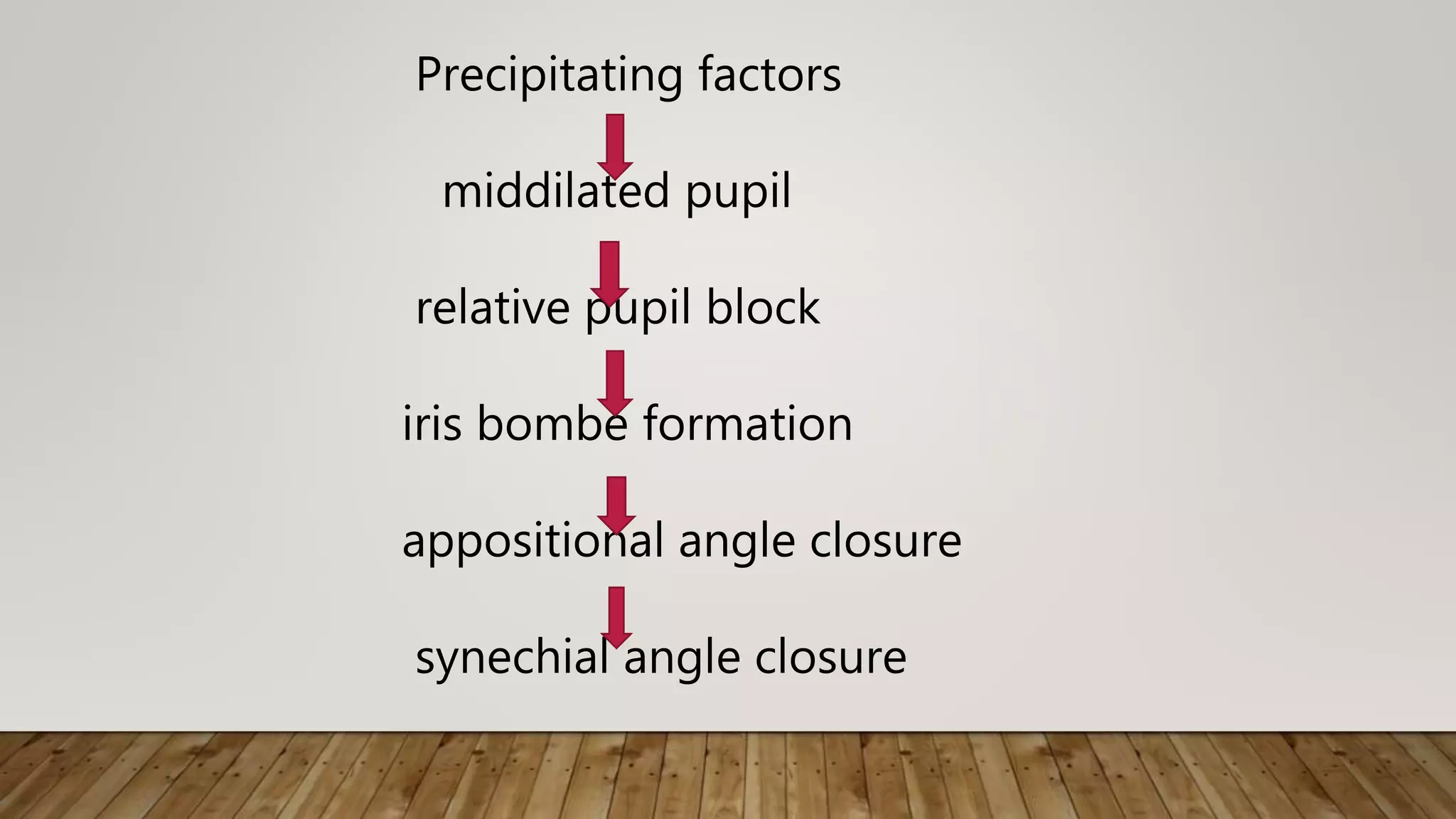
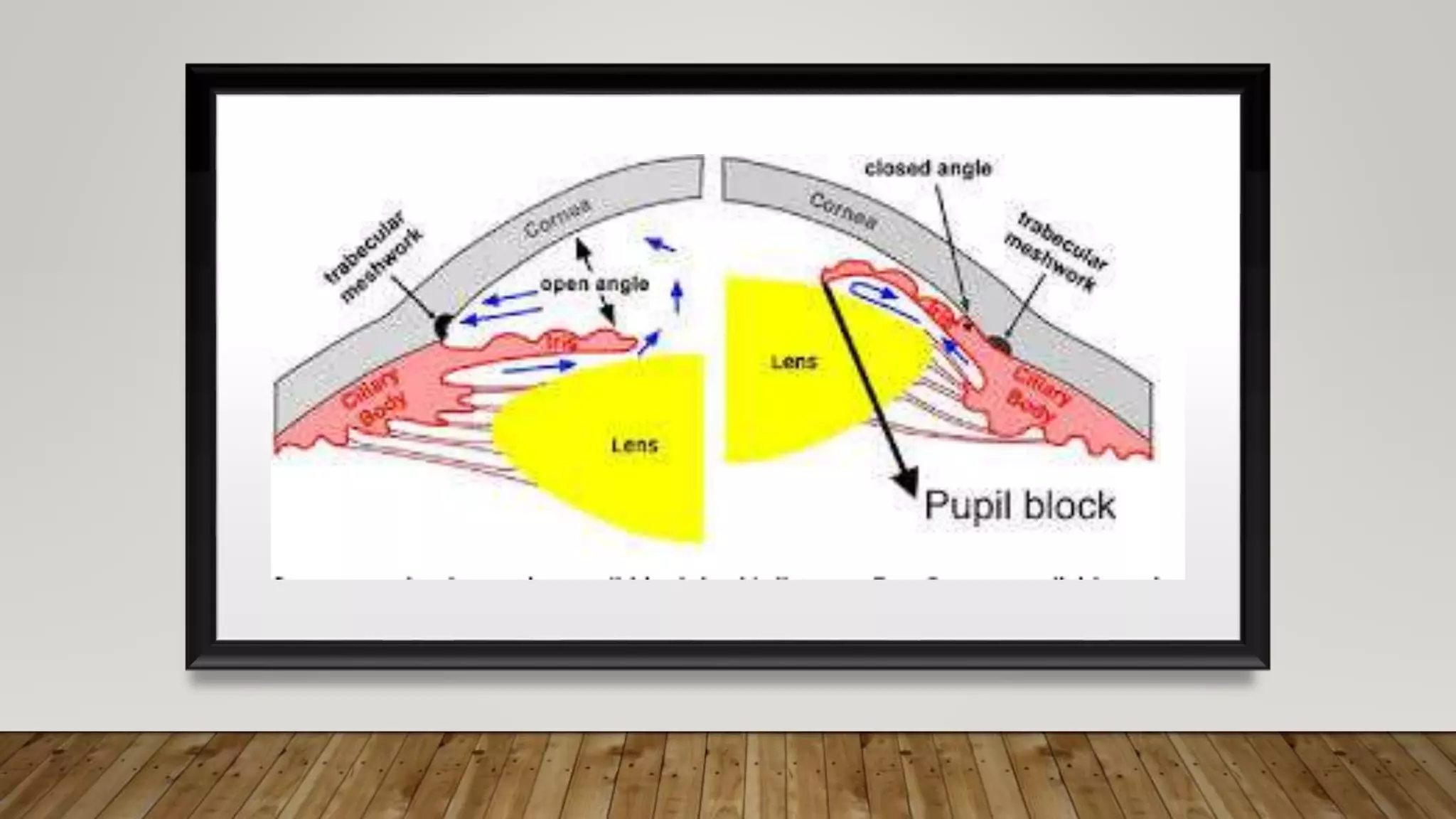
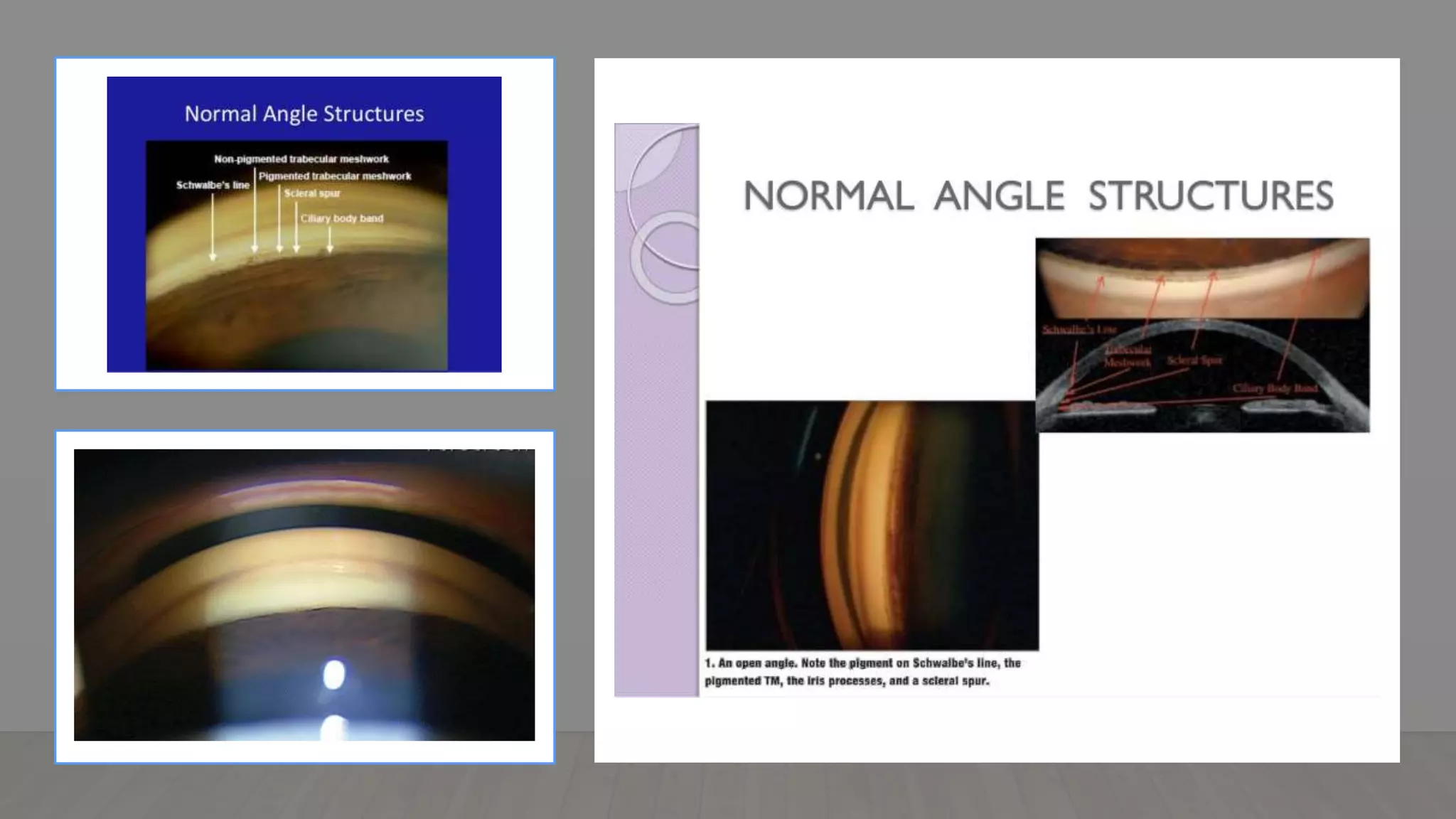
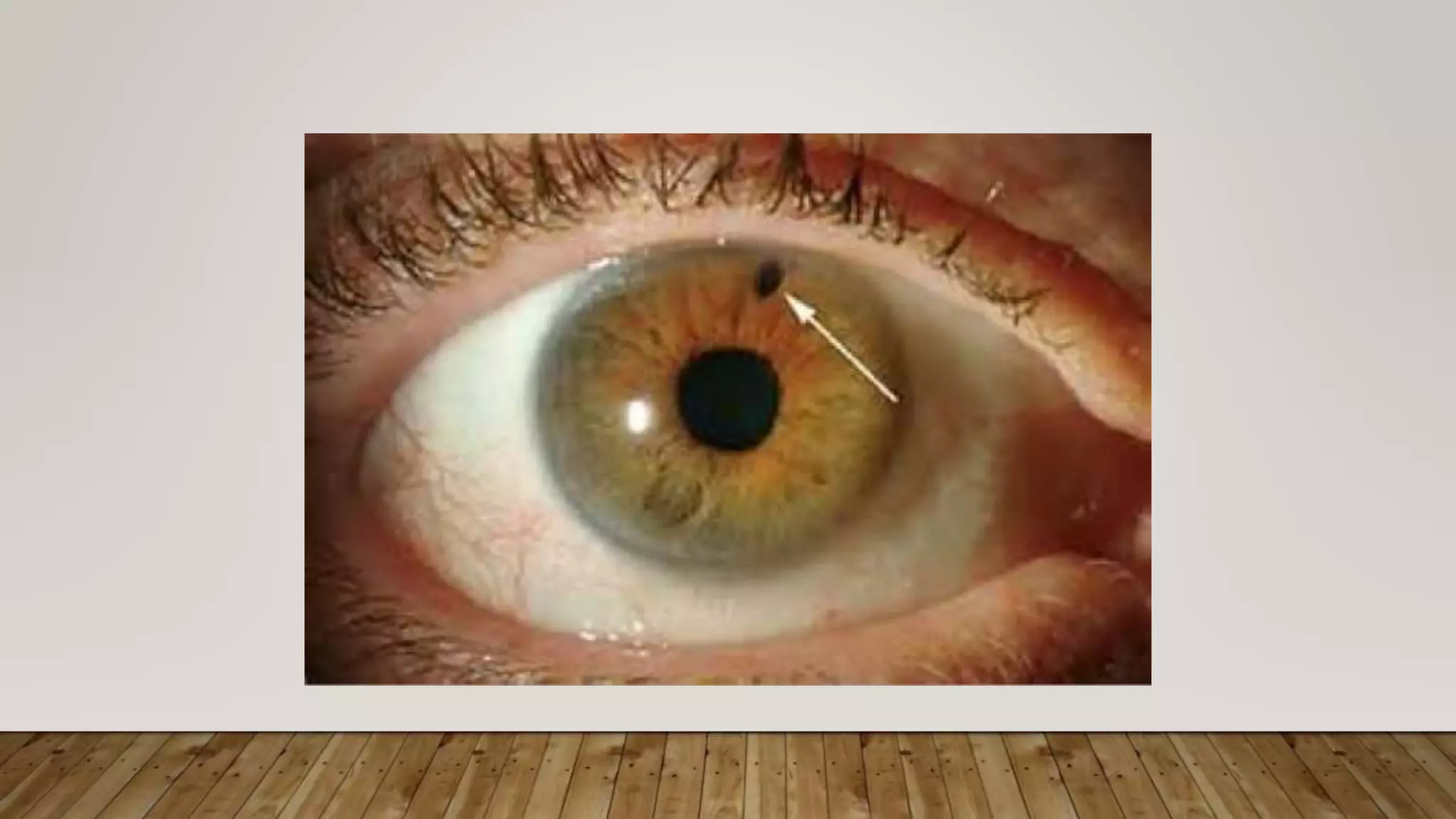
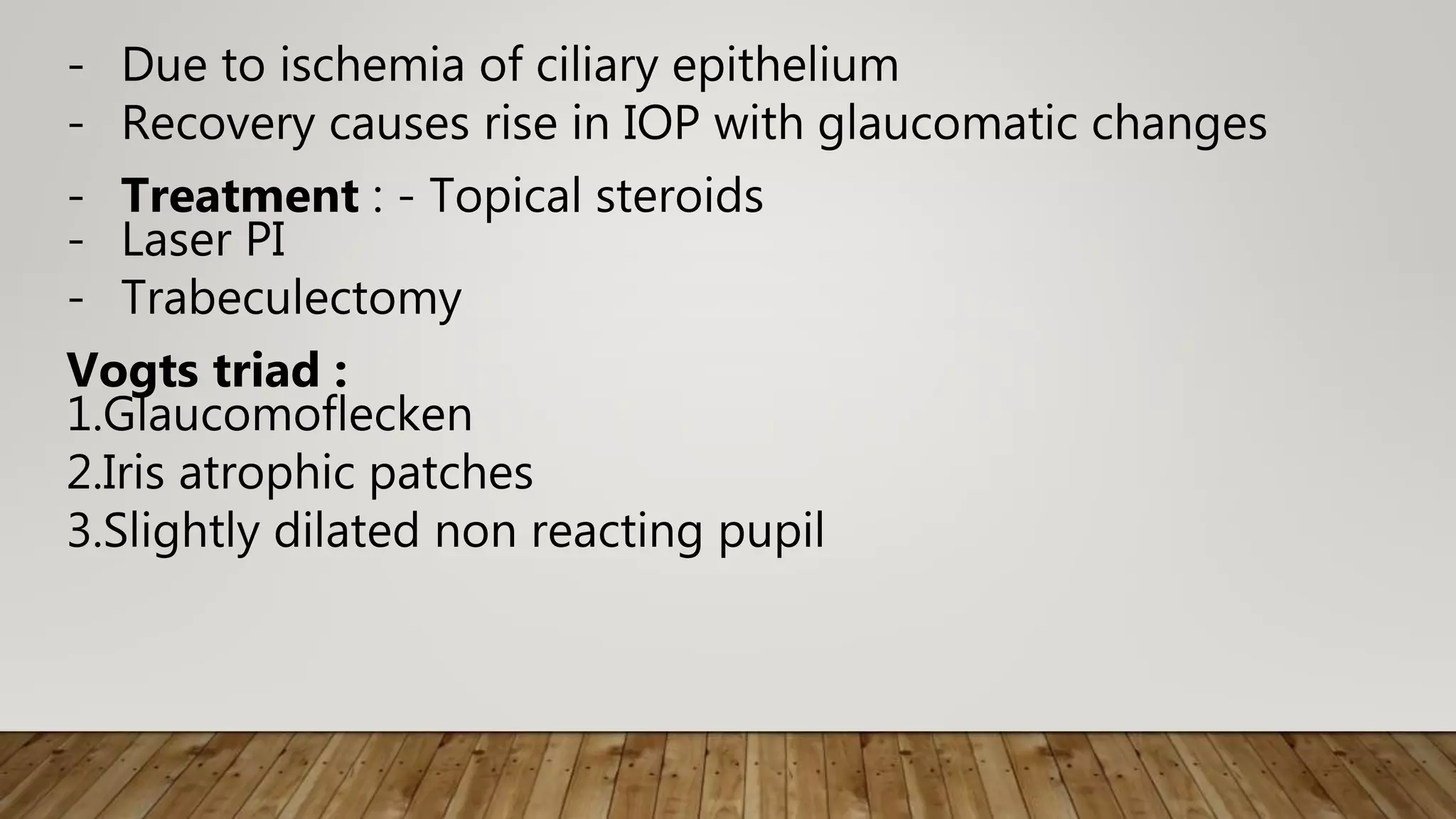
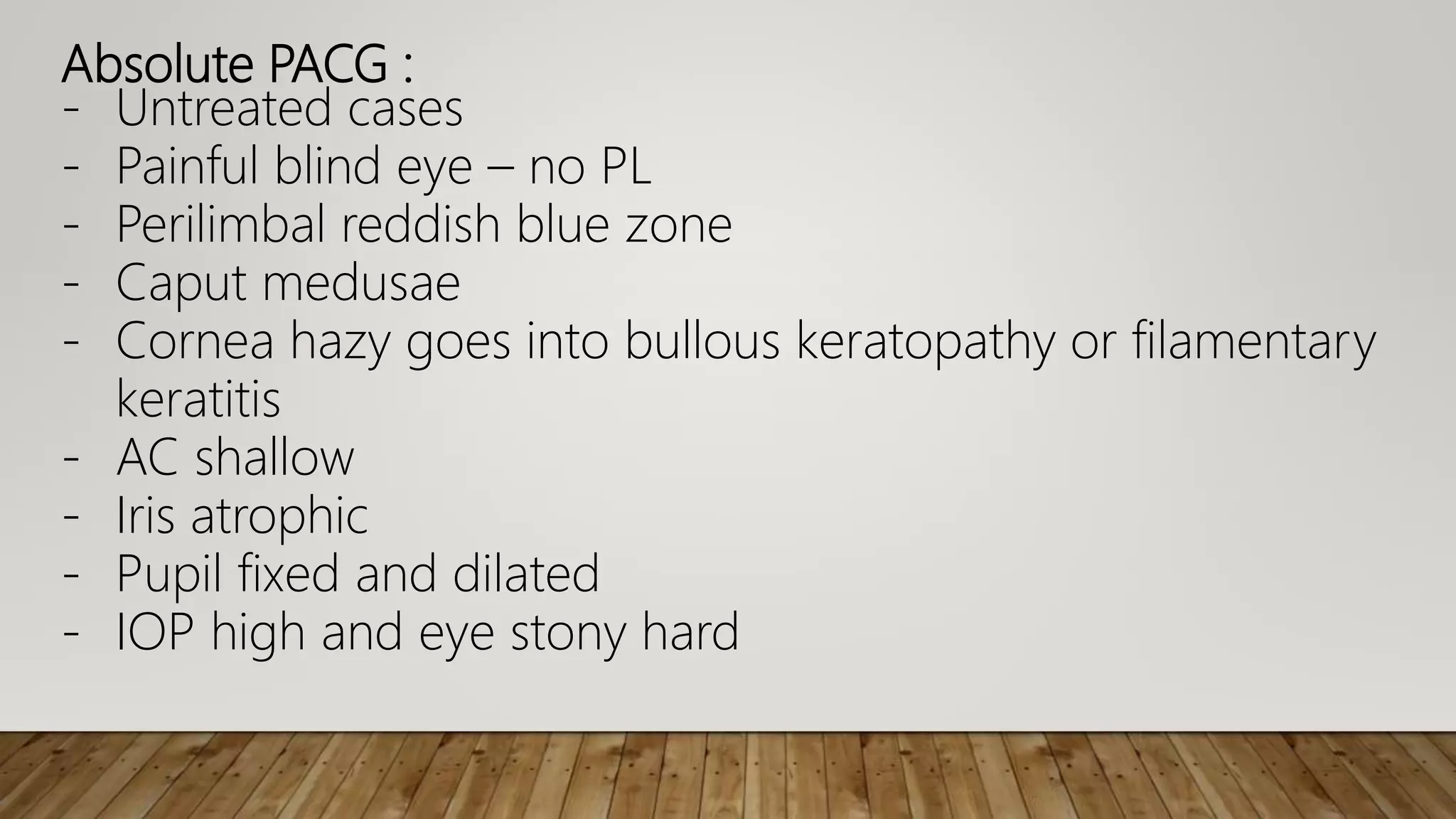
Primary angle closure glaucoma is caused by apposition of the peripheral iris against the trabecular meshwork, obstructing aqueous outflow. It is a major cause of glaucoma blindness worldwide. Risk factors include older age, female sex, Southeast Asian or Chinese descent, hyperopia, anatomically narrow anterior chamber angles, and heredity. Primary angle closure can progress to primary angle closure glaucoma if untreated, causing increased intraocular pressure and optic nerve damage. Treatment options include laser peripheral iridotomy, medications, filtration surgery, and lens extraction depending on the stage and severity of the condition.