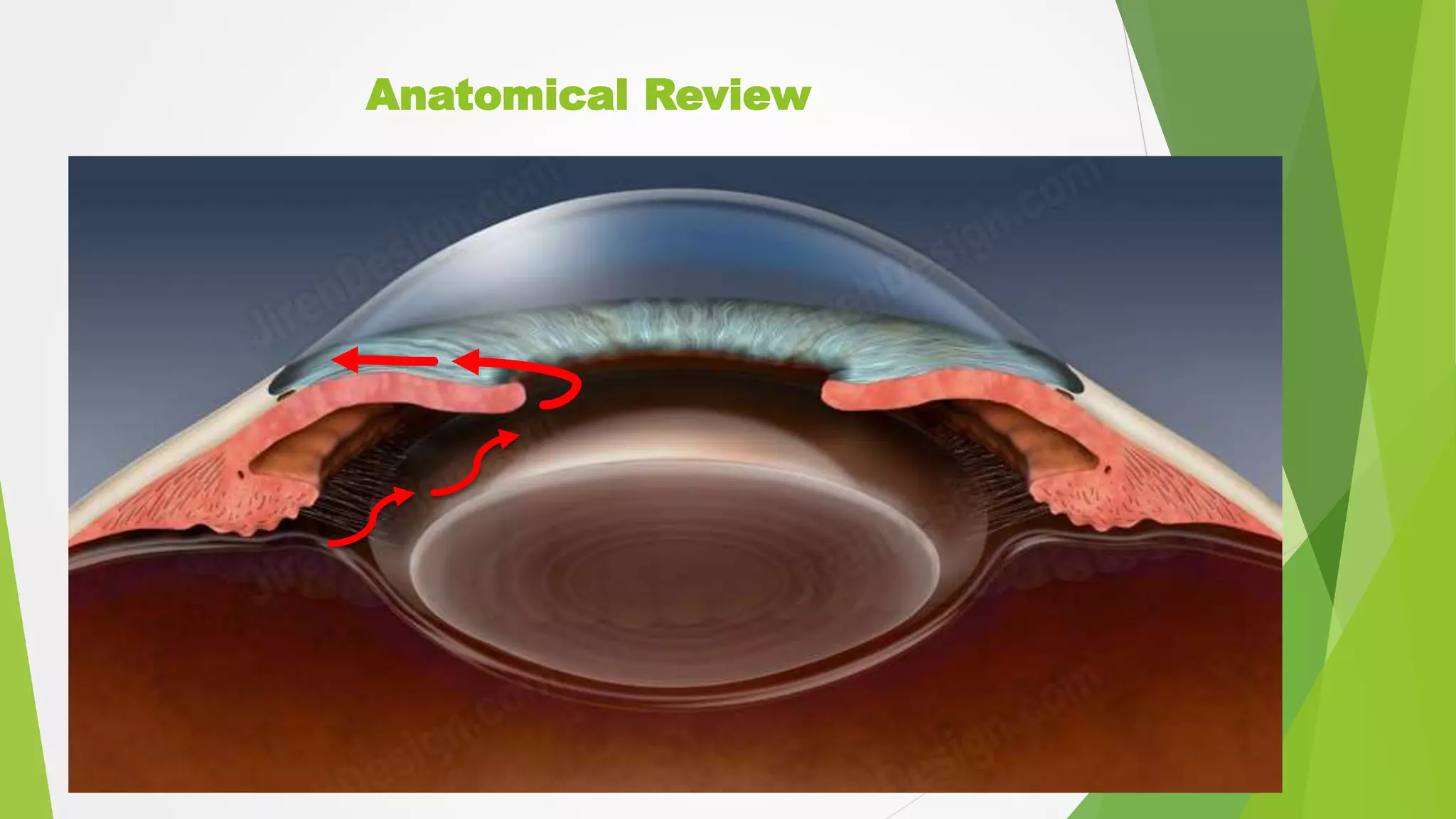
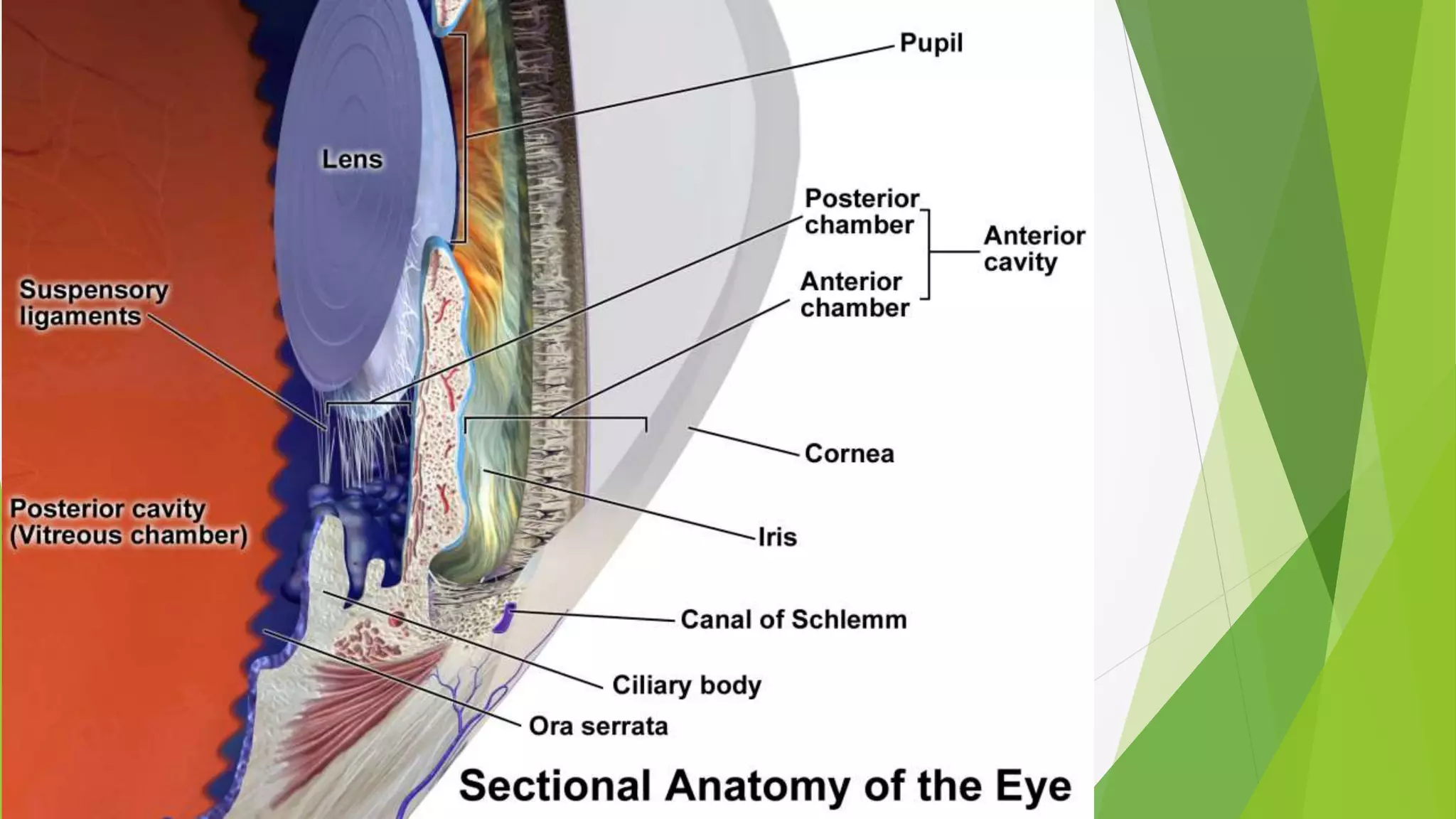
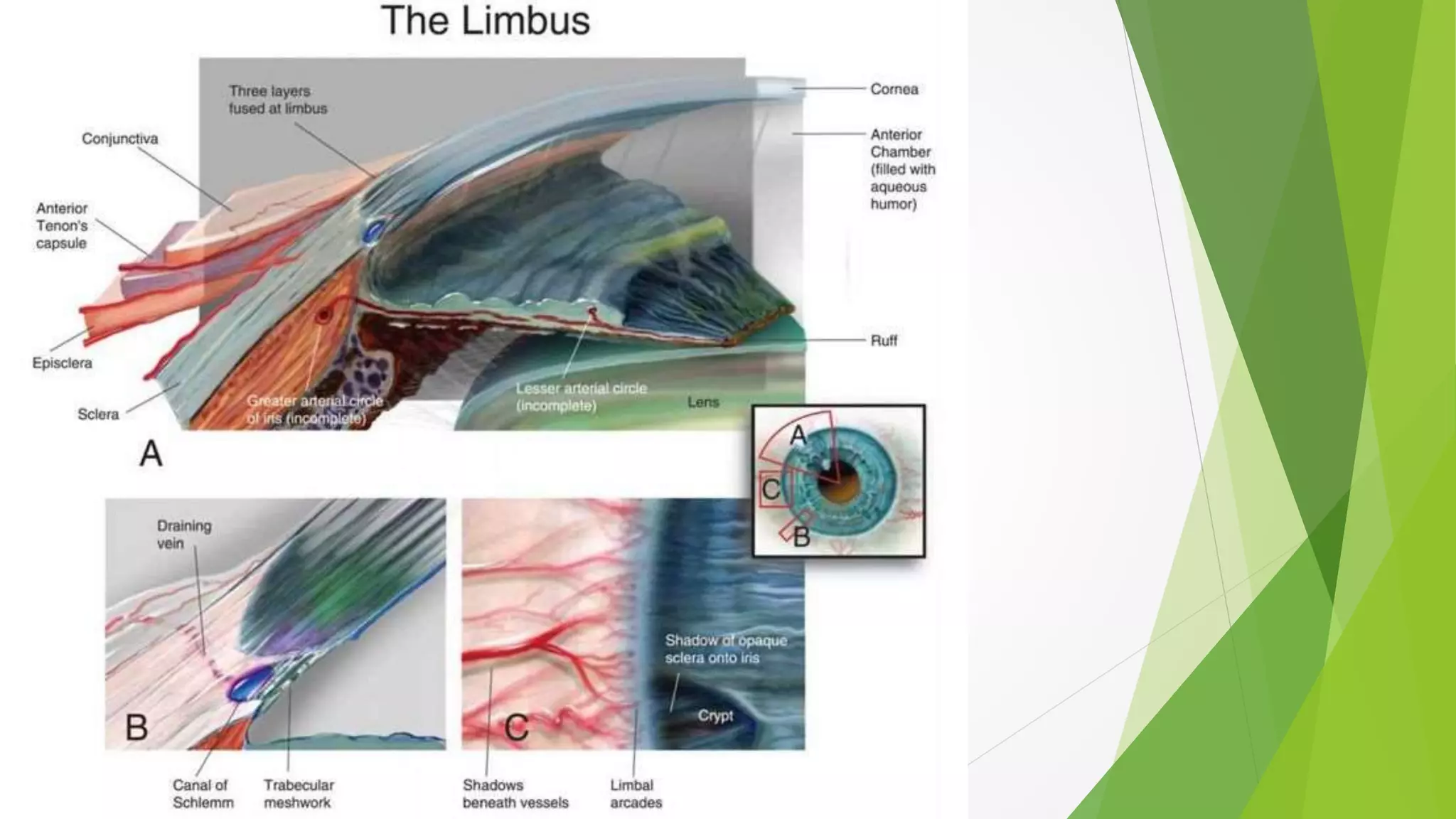
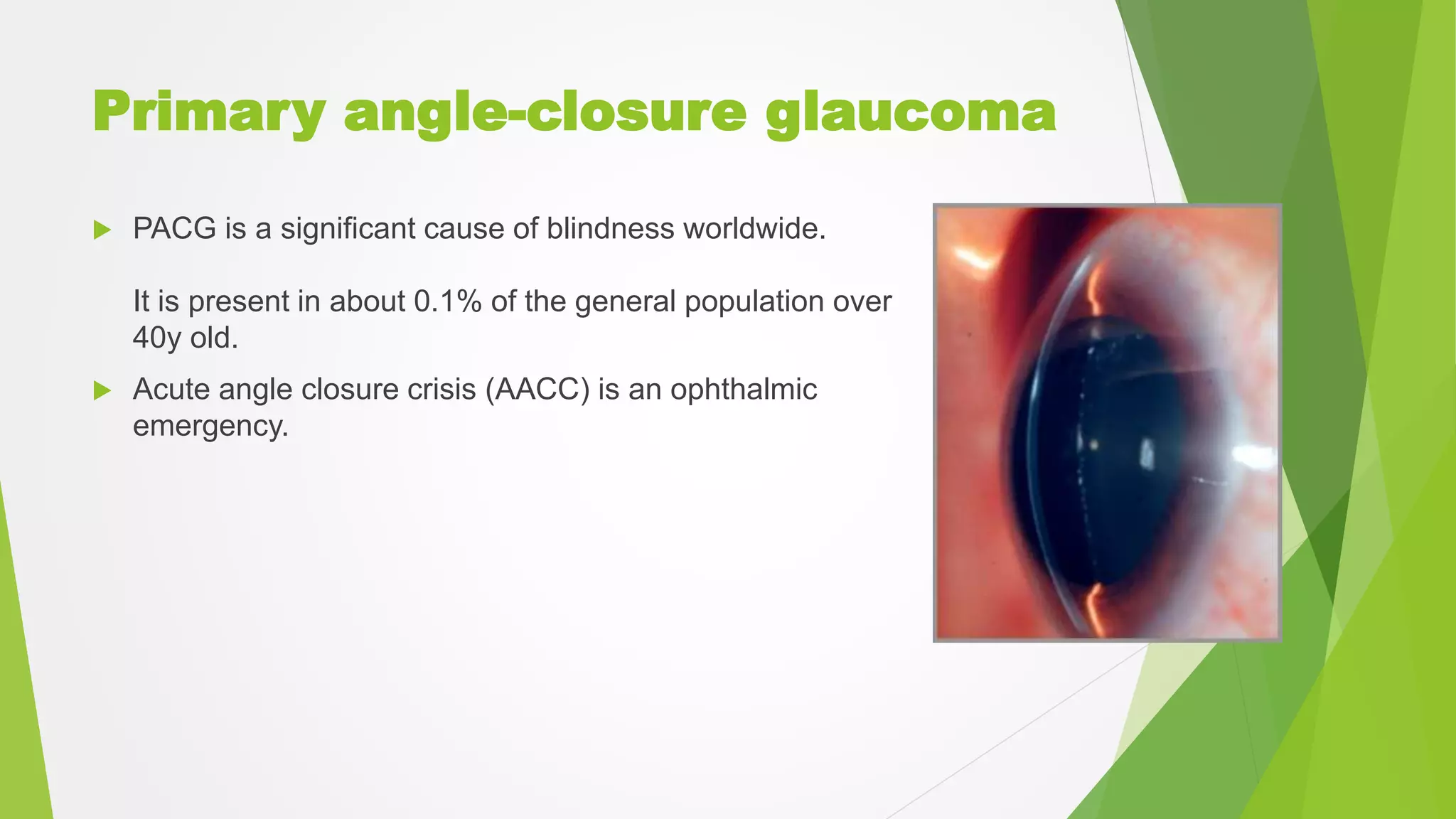
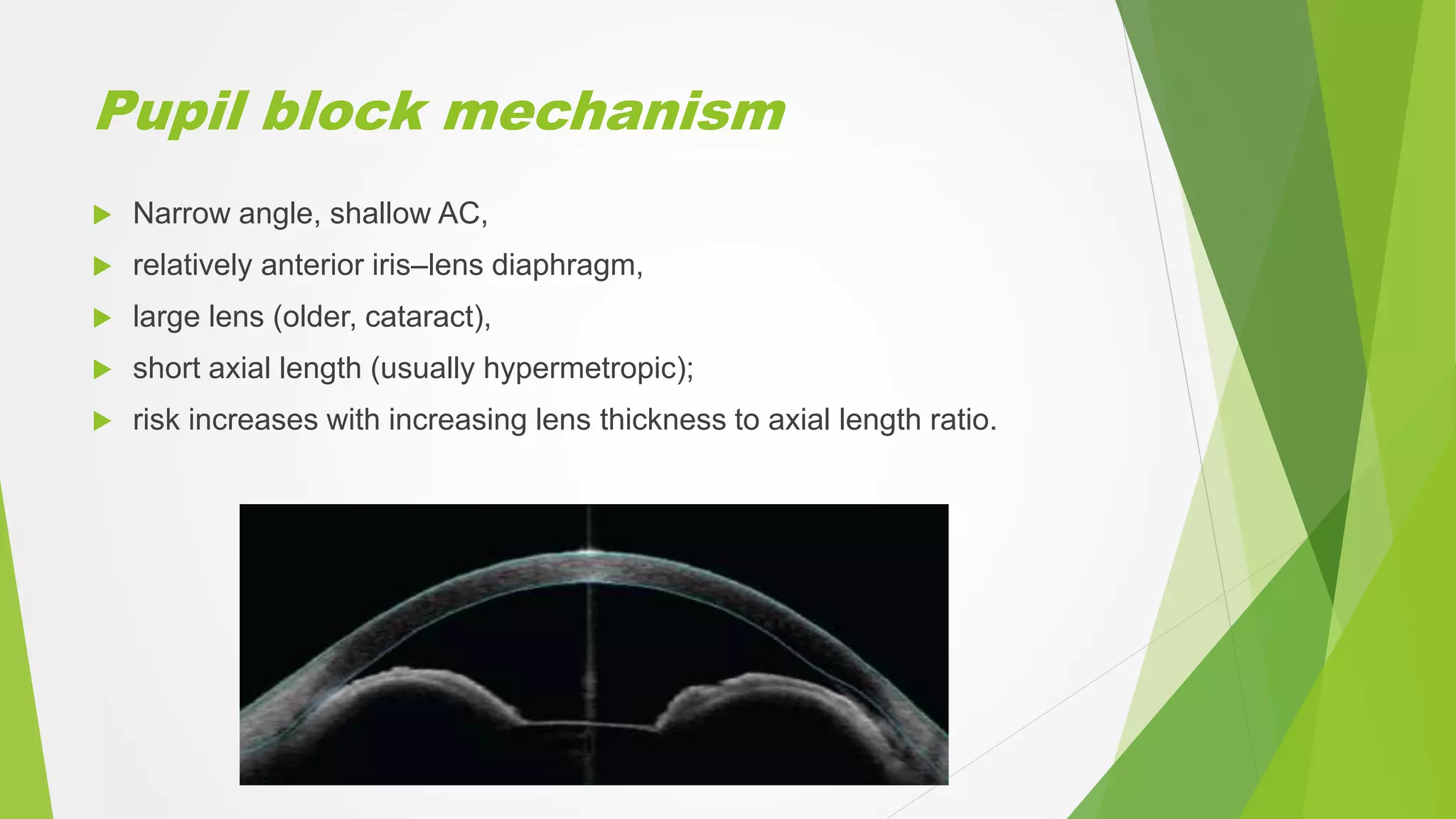
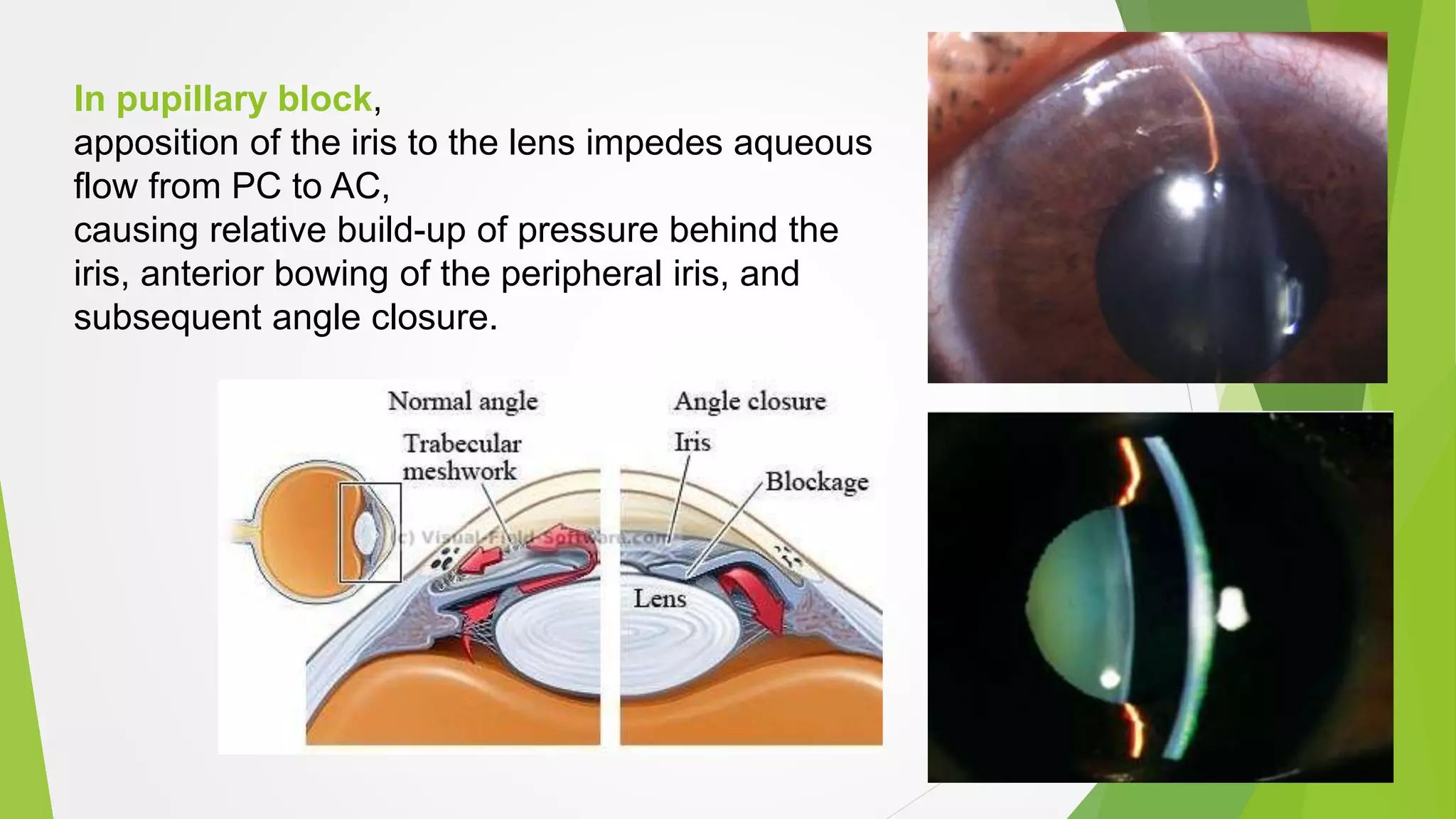
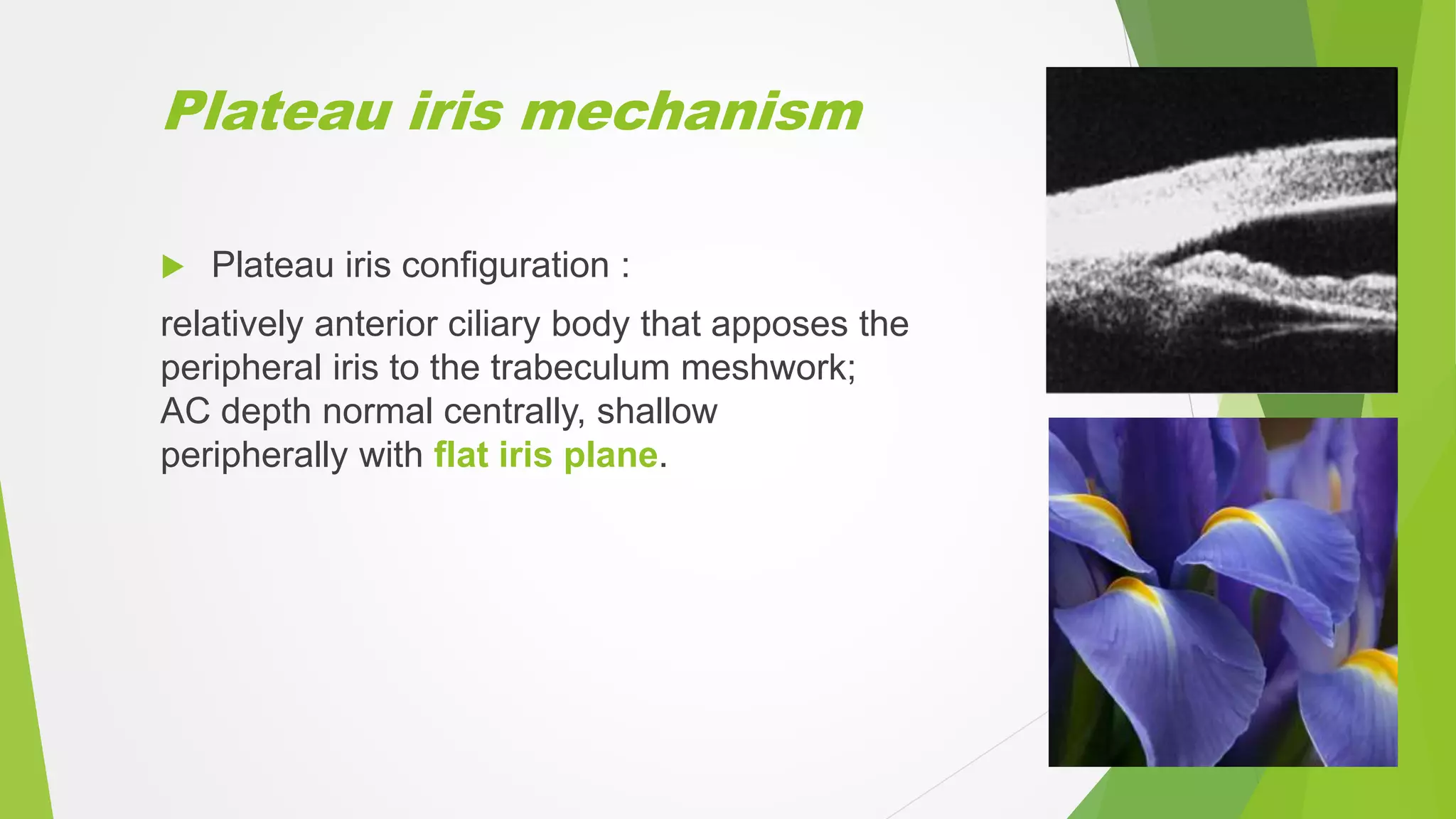
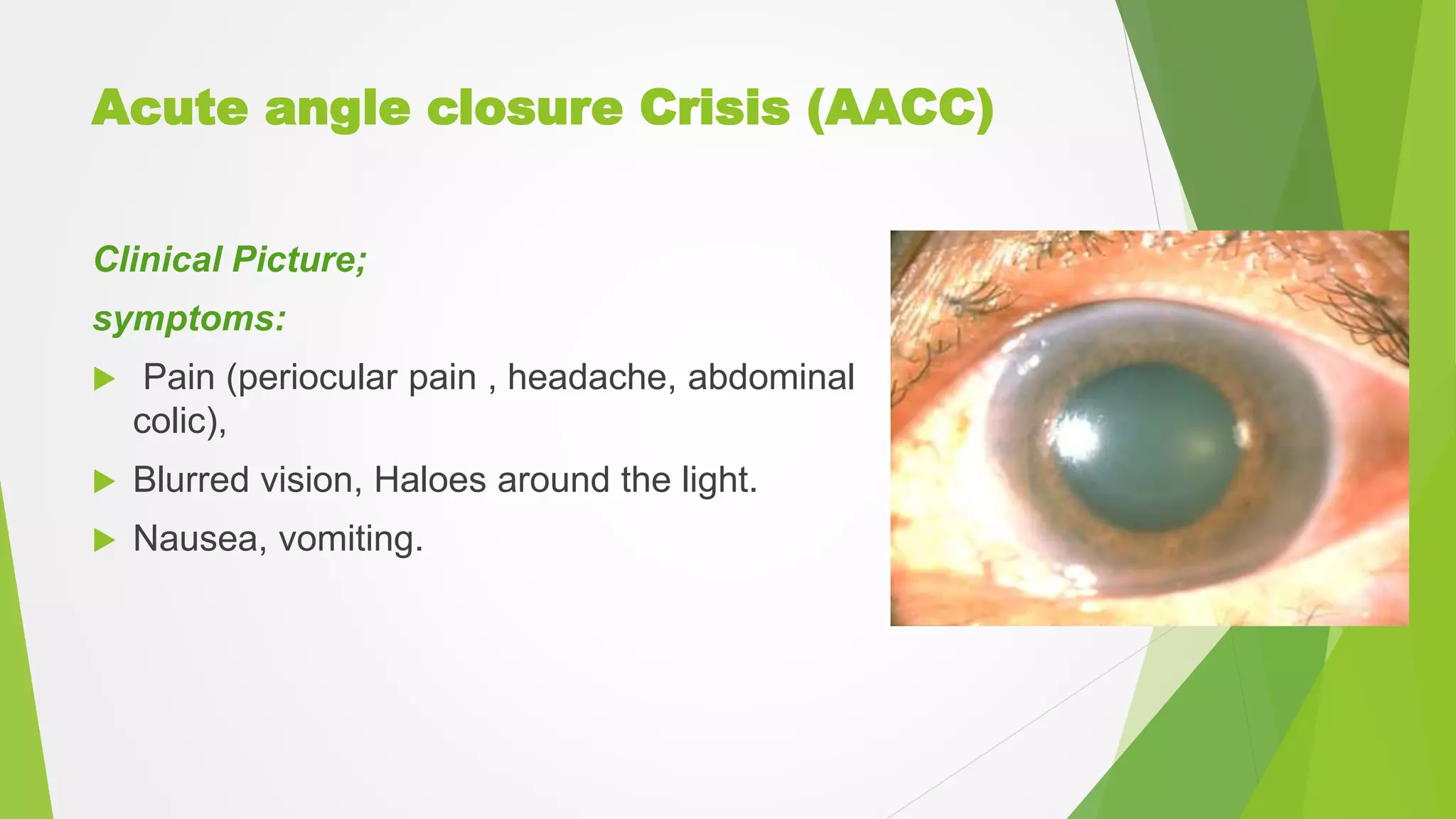
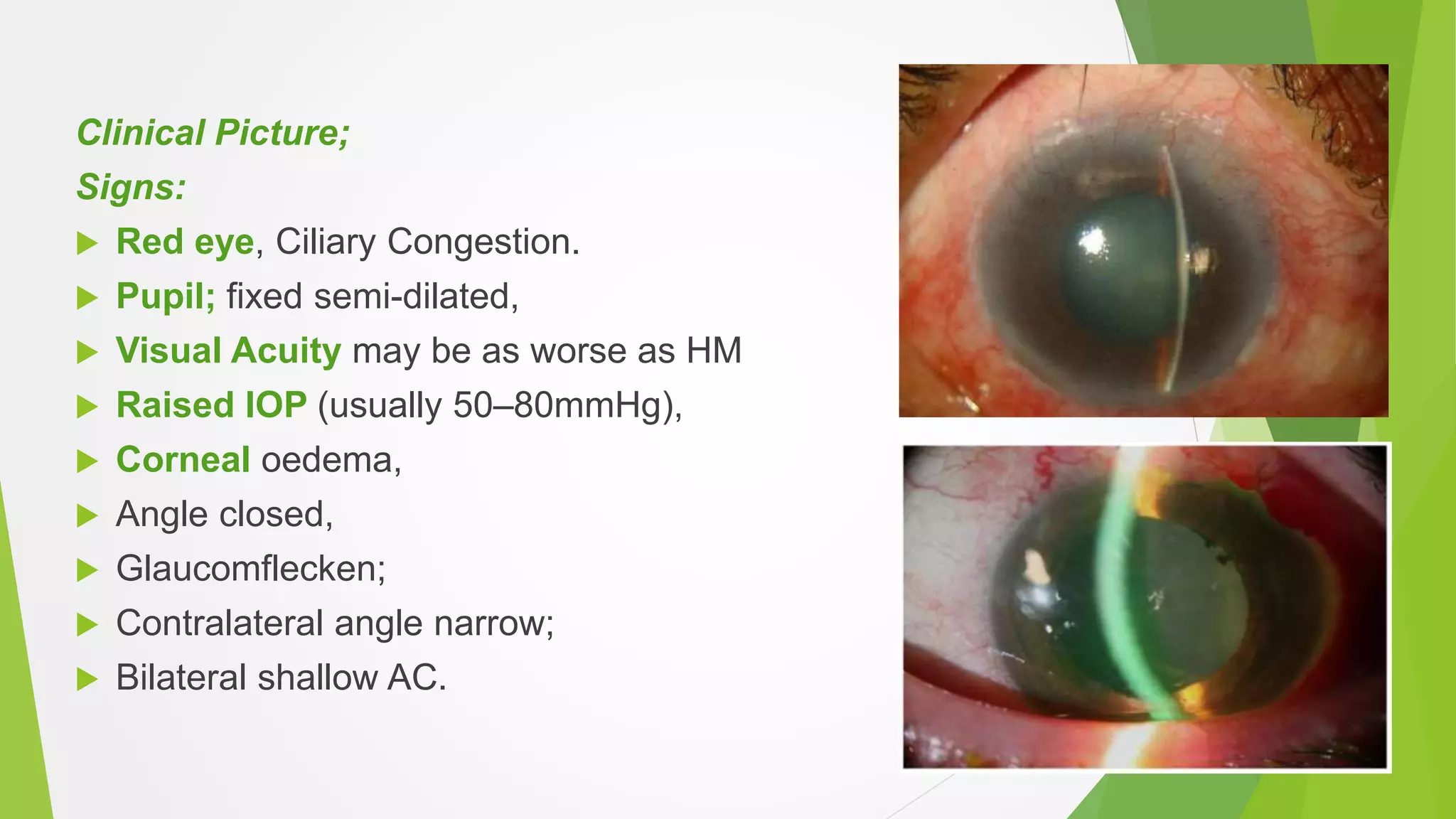
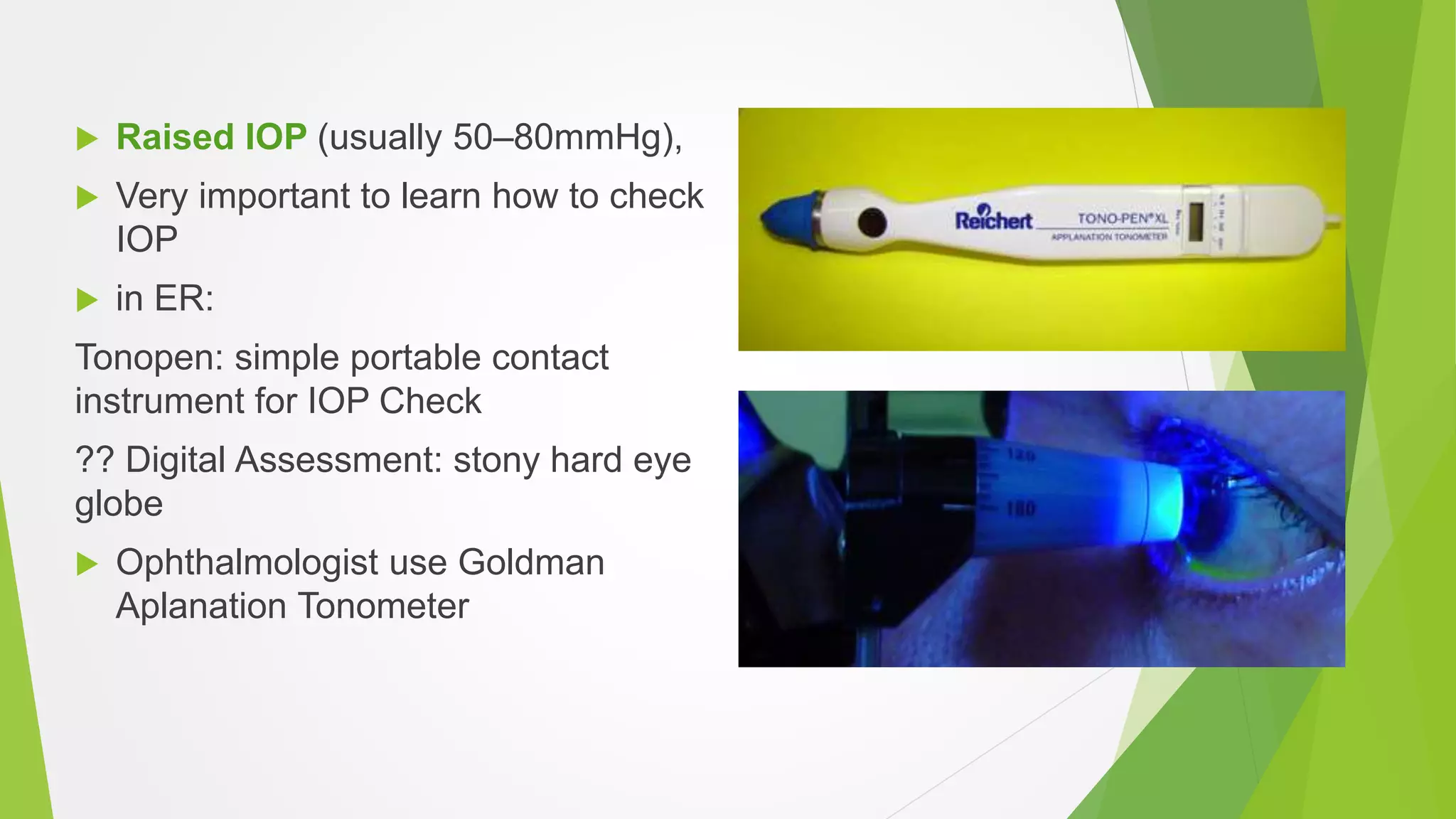
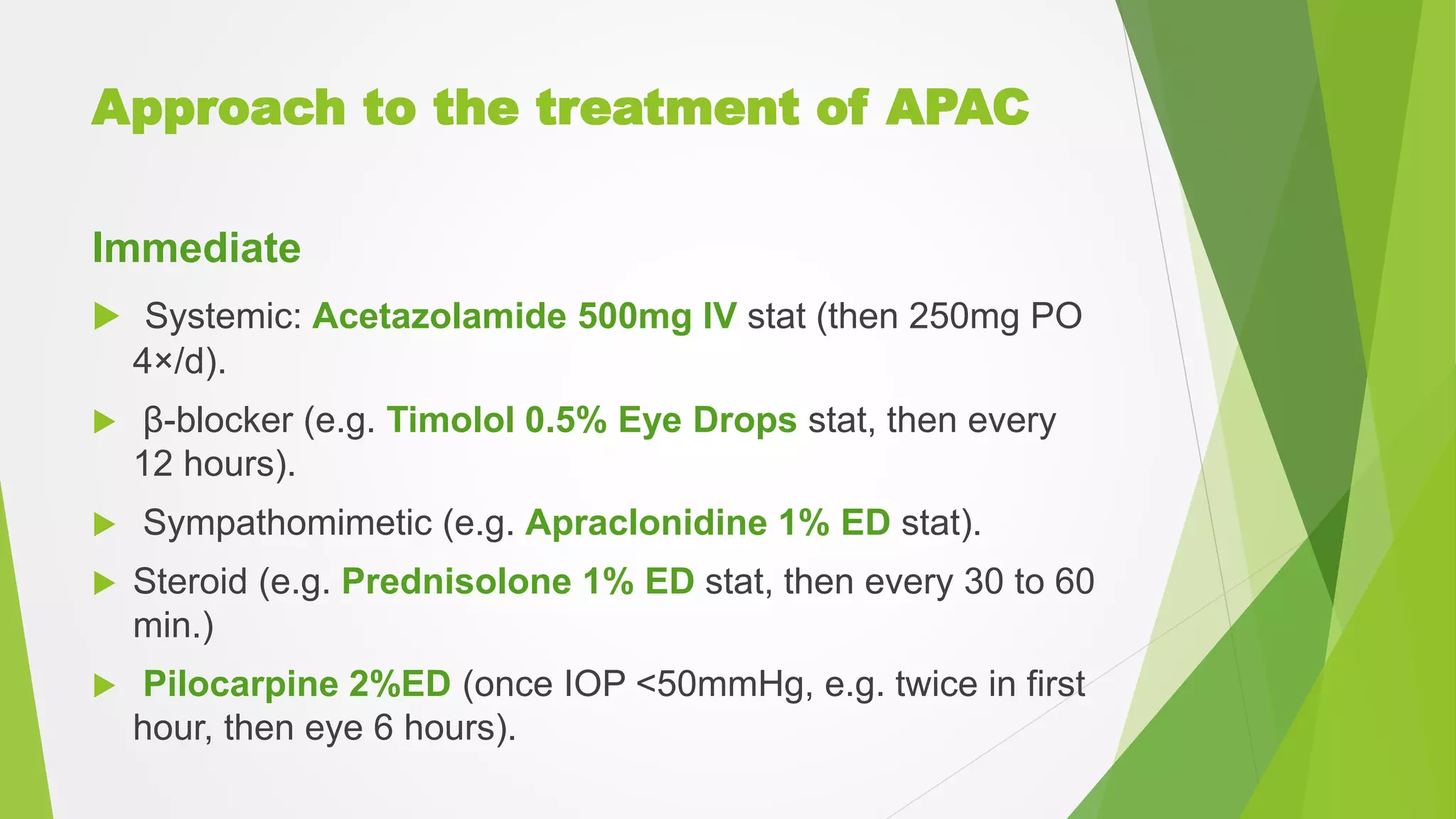
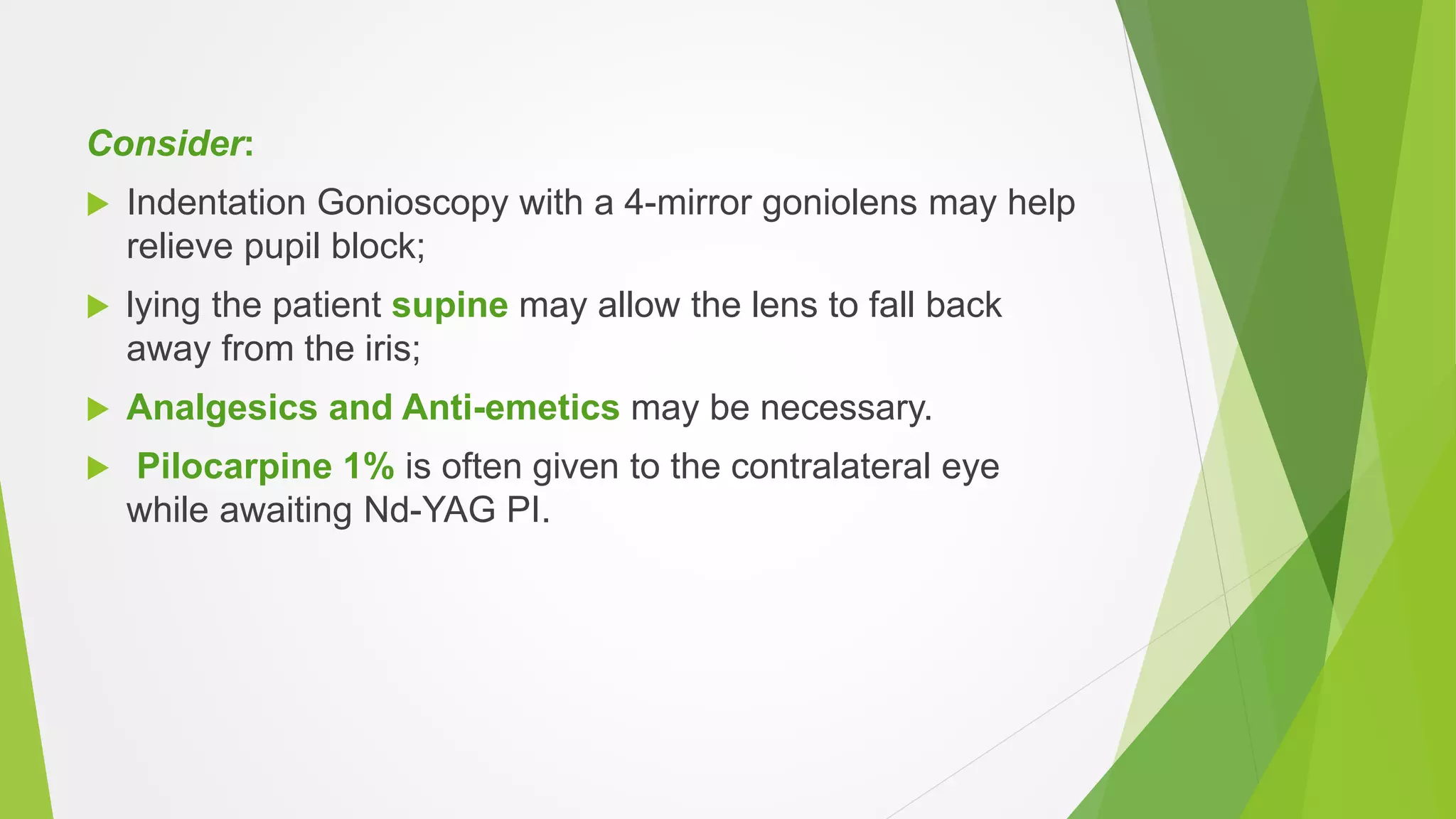
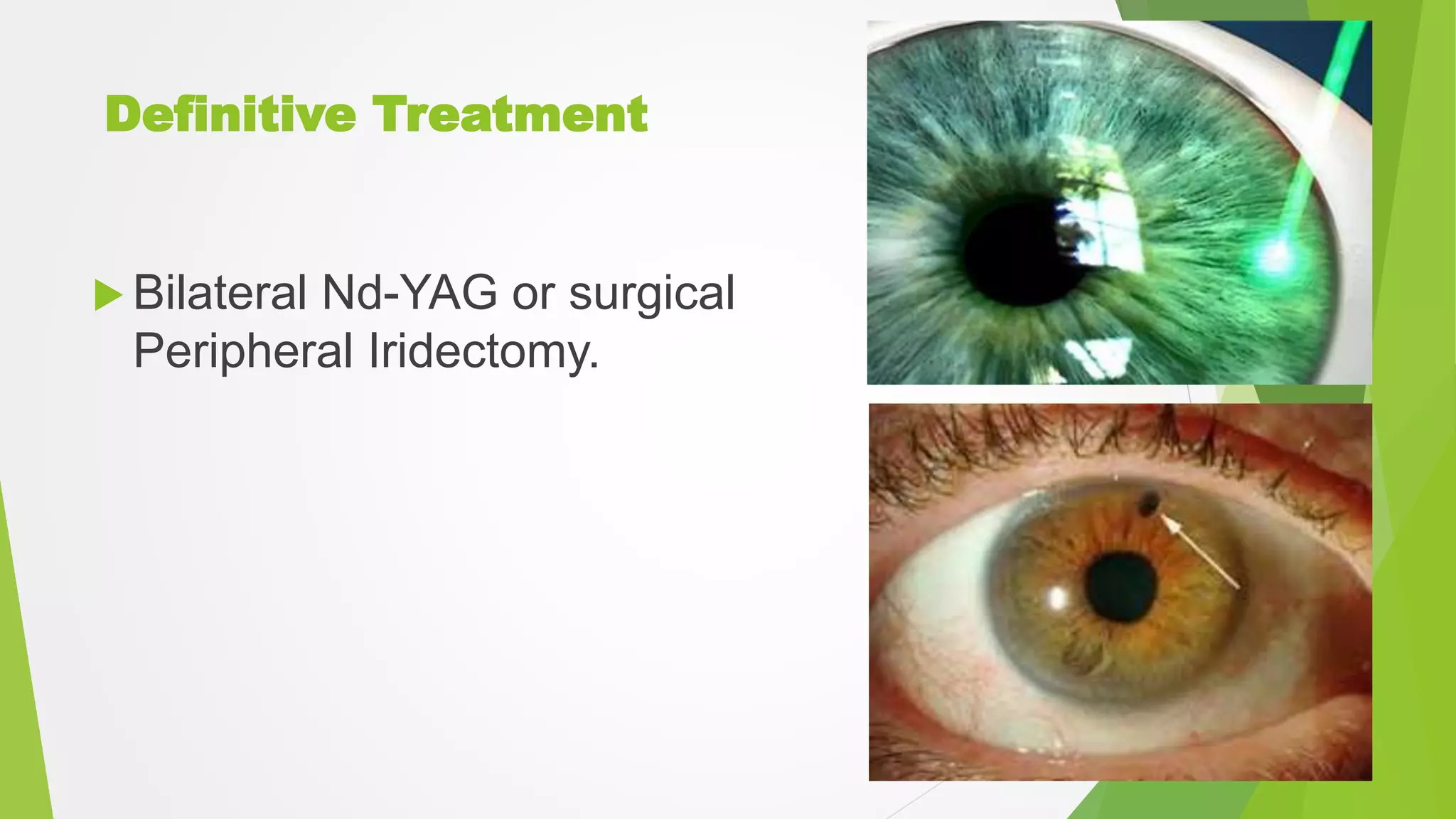
Acute angle closure crisis is an ophthalmic emergency caused by sudden rise in intraocular pressure due to blockage of aqueous outflow. It presents with severe eye pain, blurred vision, nausea and elevated eye pressure. Immediate treatment involves intravenous acetazolamide and topical eye drops to lower pressure. If pressure is not controlled, further interventions like laser iridotomy or surgery may be needed to relieve the block and prevent permanent vision loss from optic nerve damage. Long term management involves treatment of the underlying primary angle closure glaucoma with pressure lowering eye drops or surgery and monitoring for glaucoma progression.