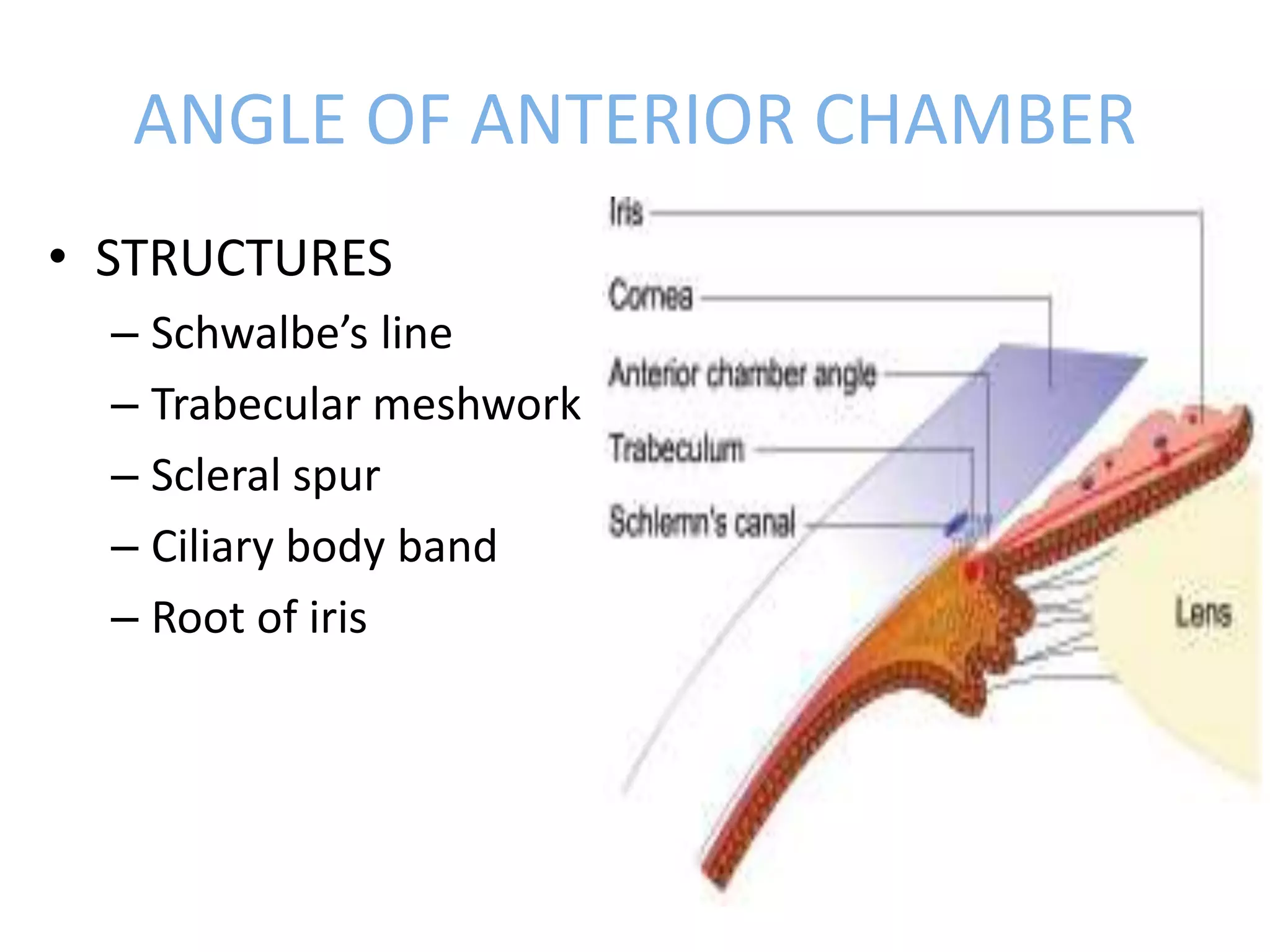
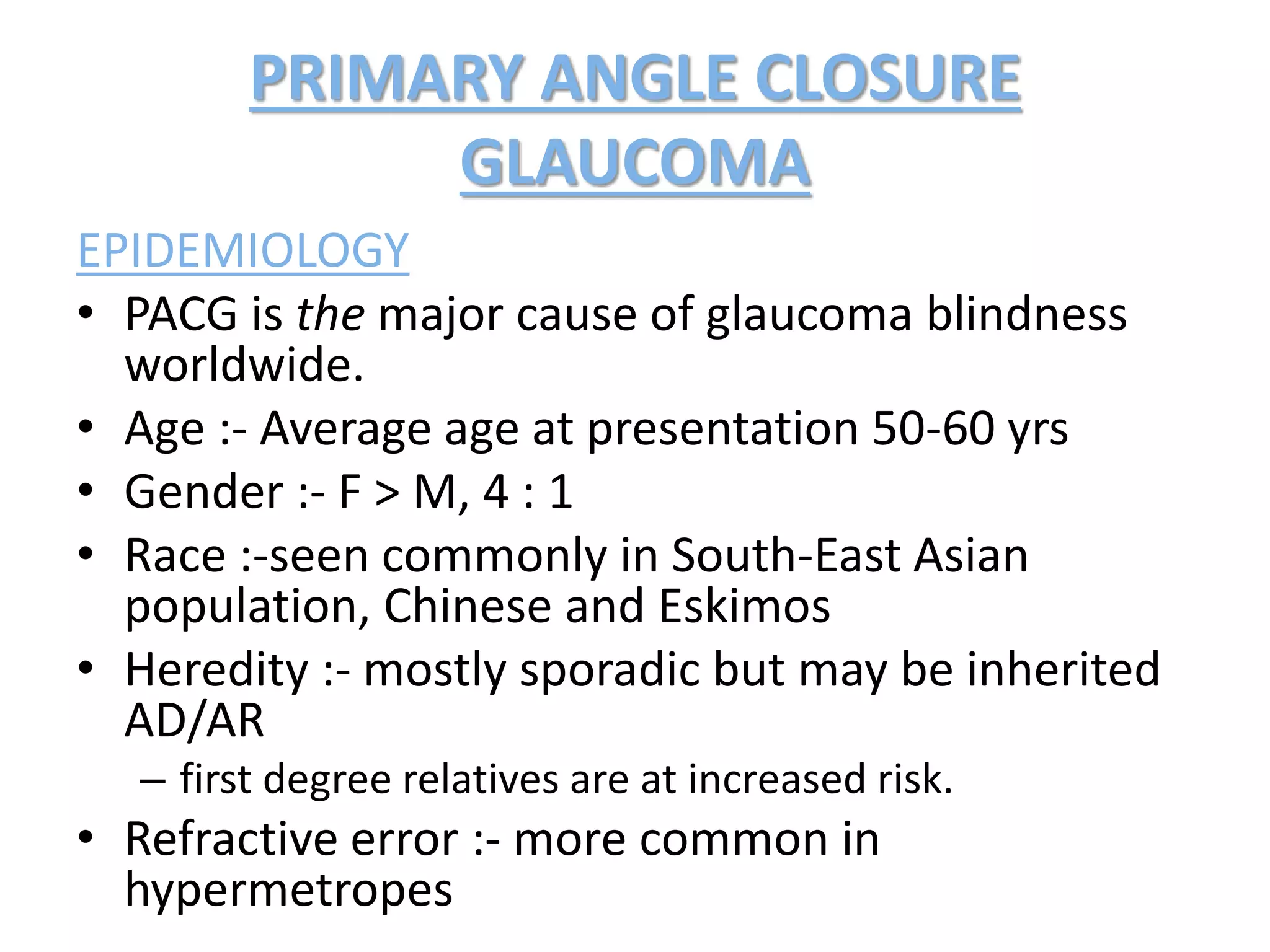
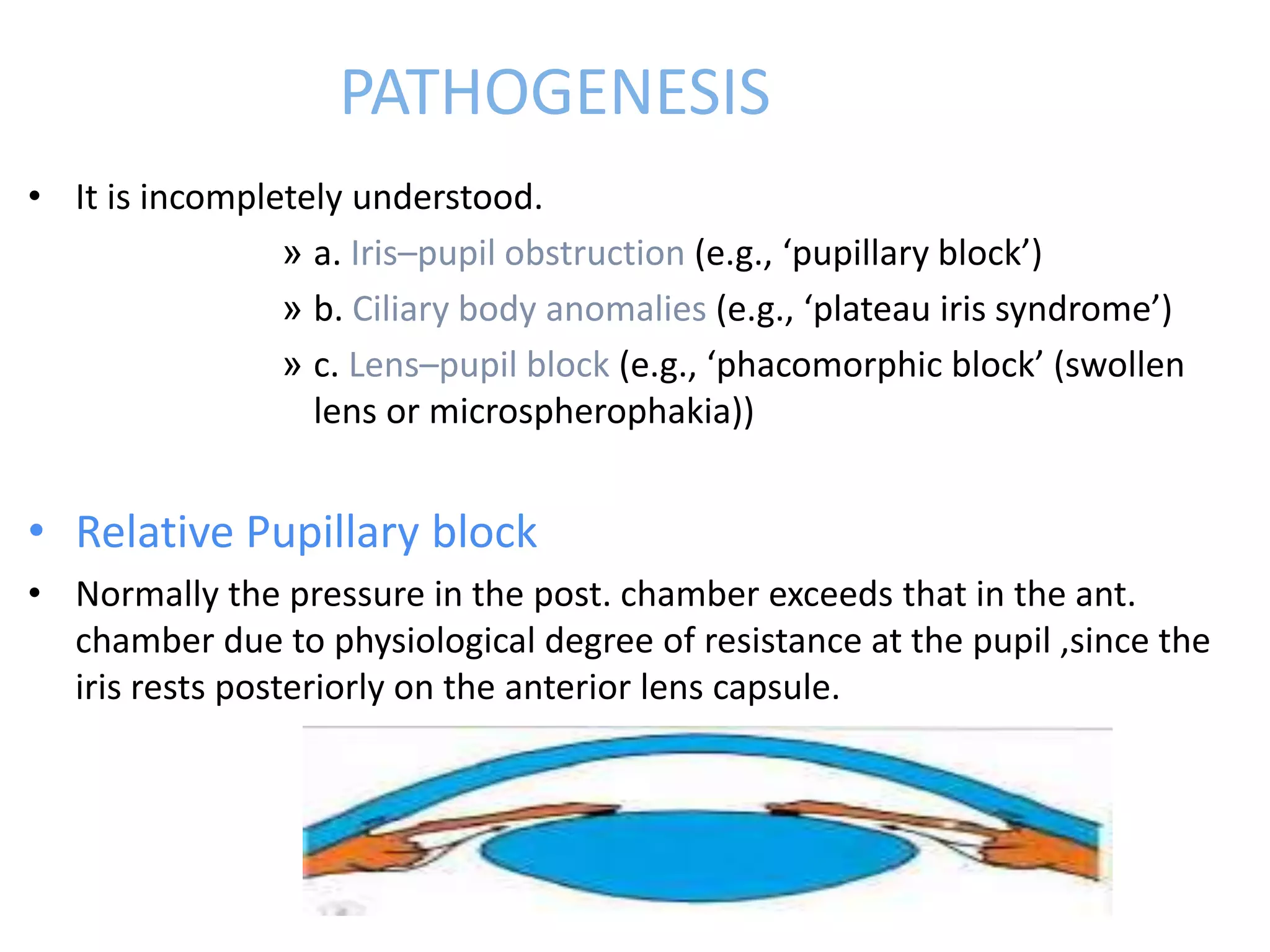
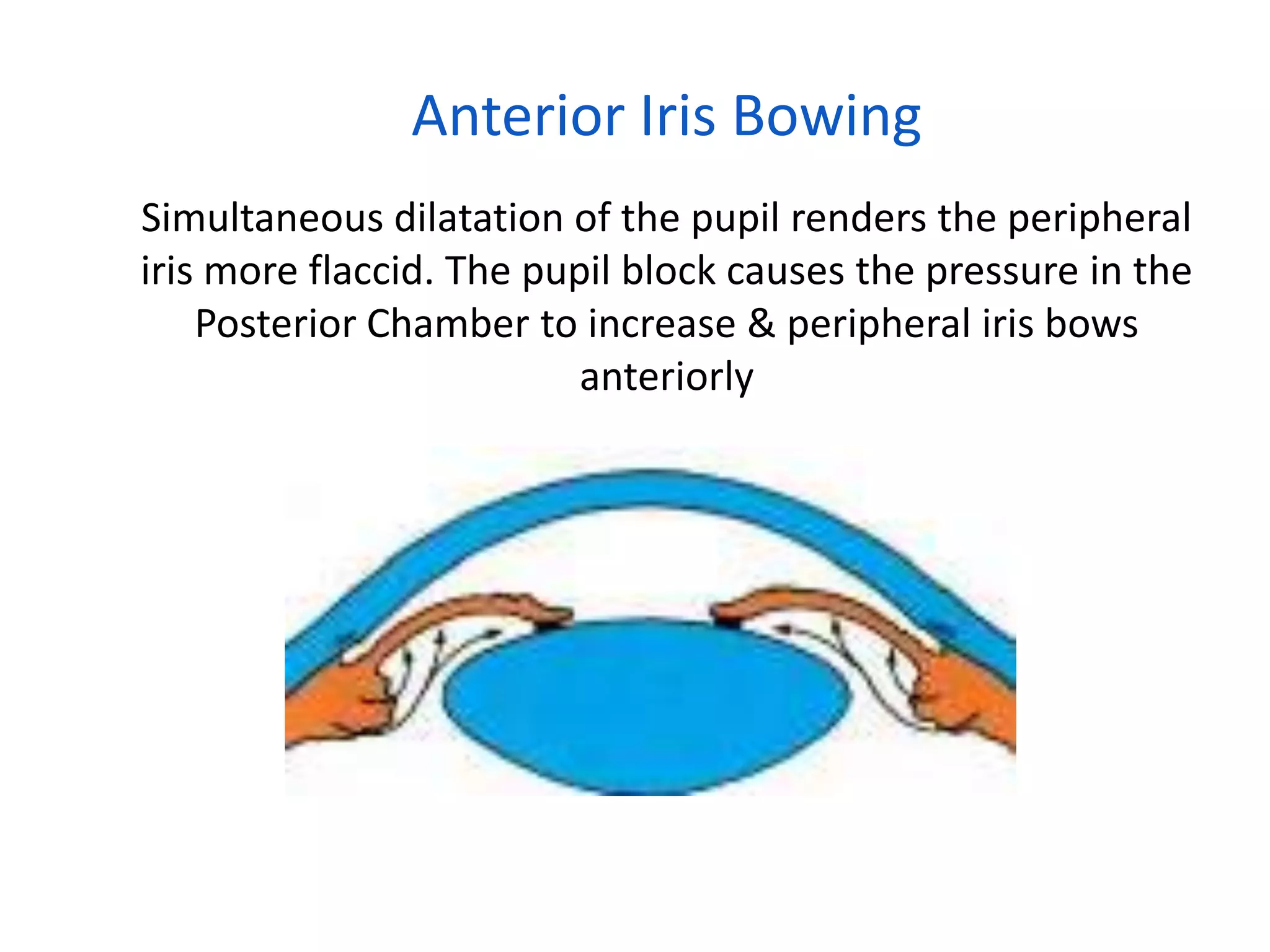
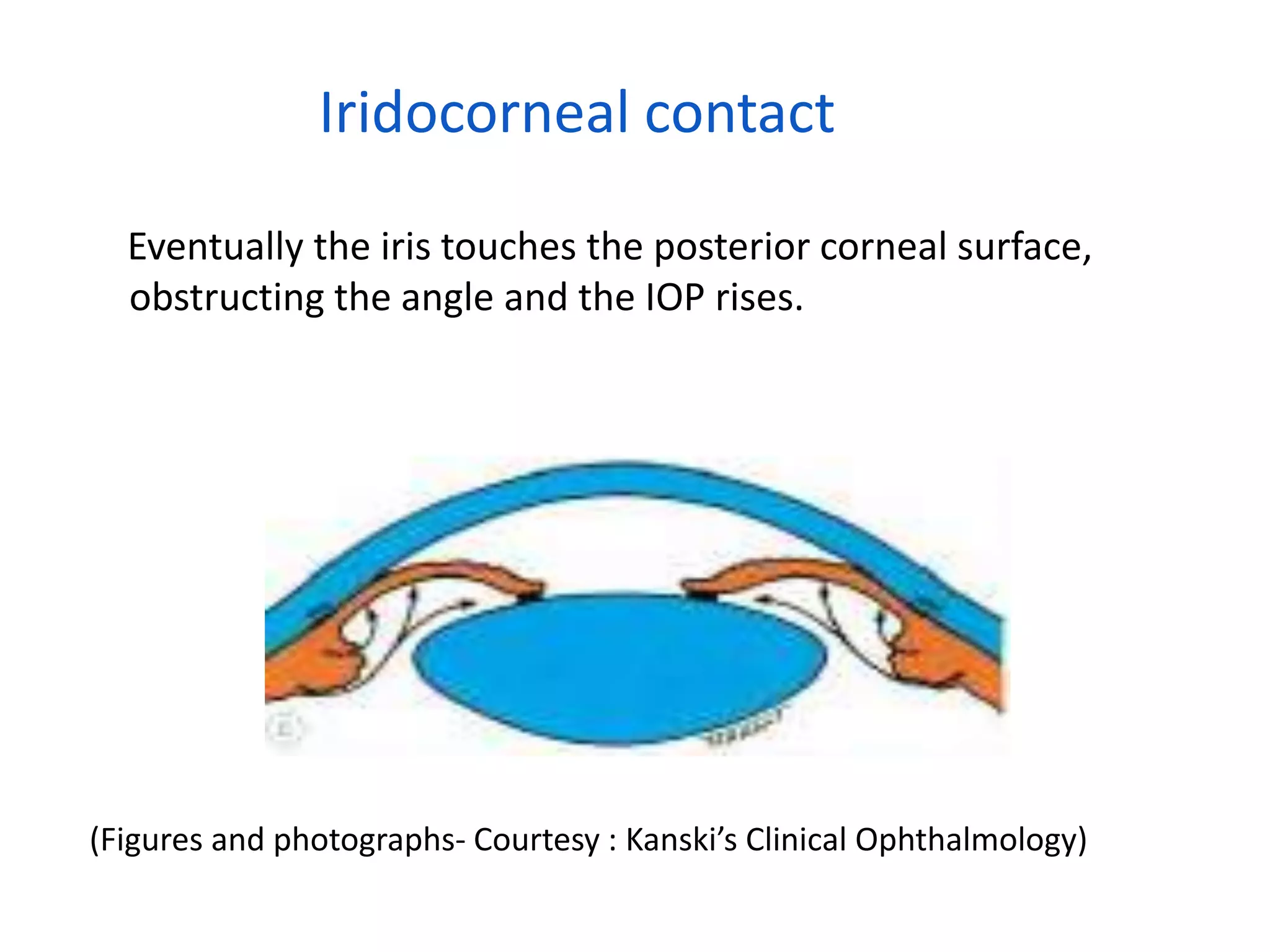
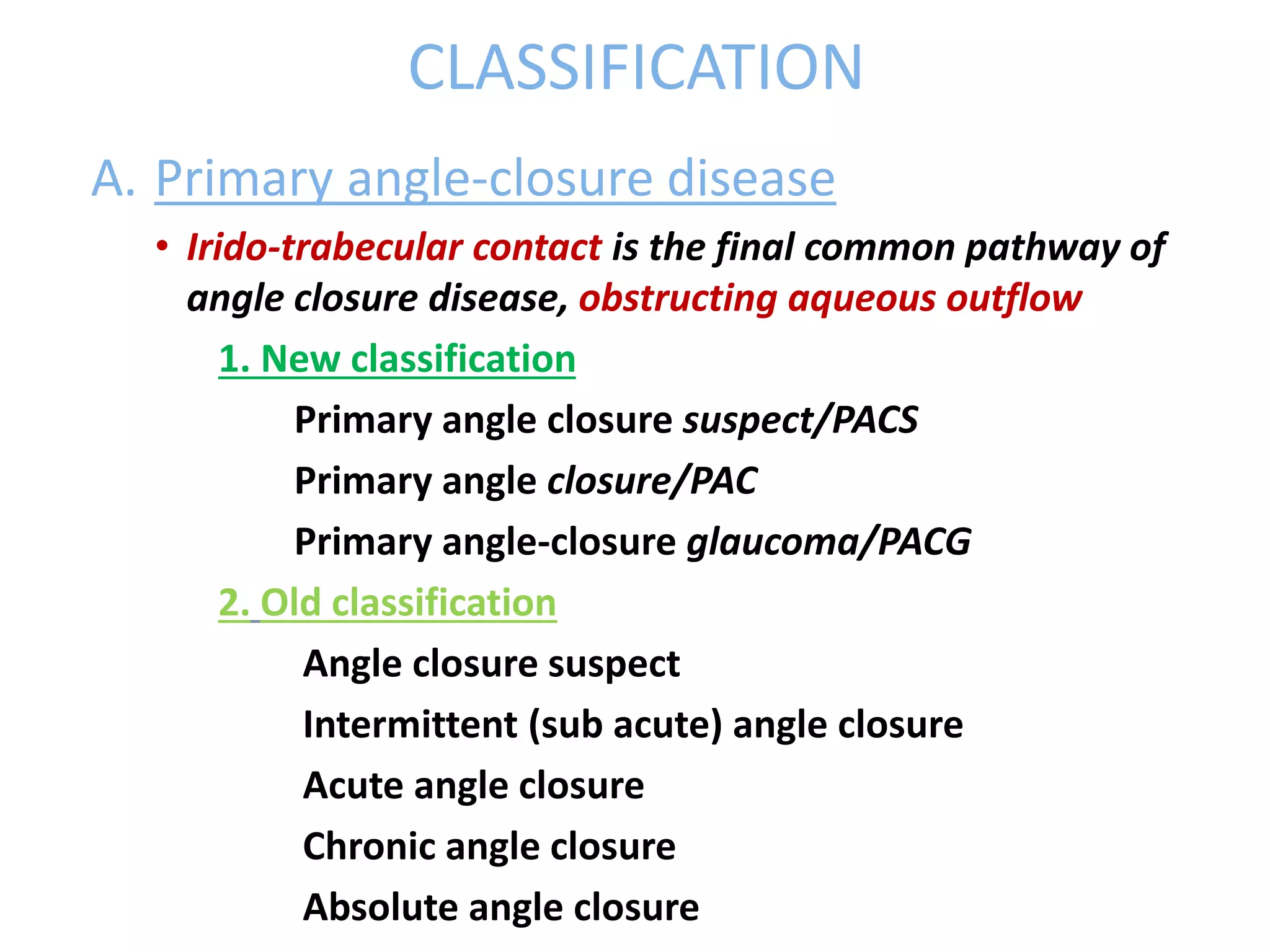
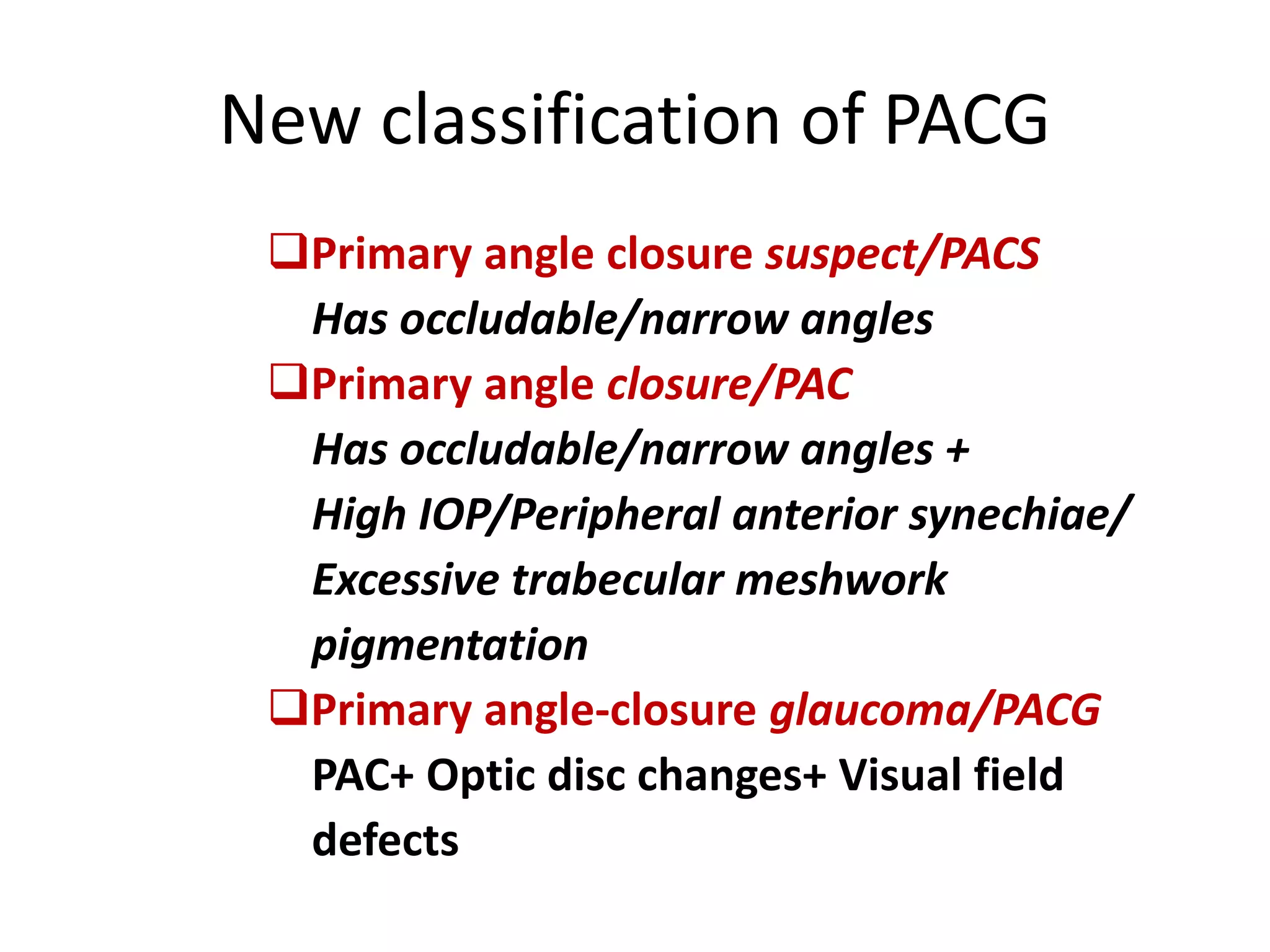
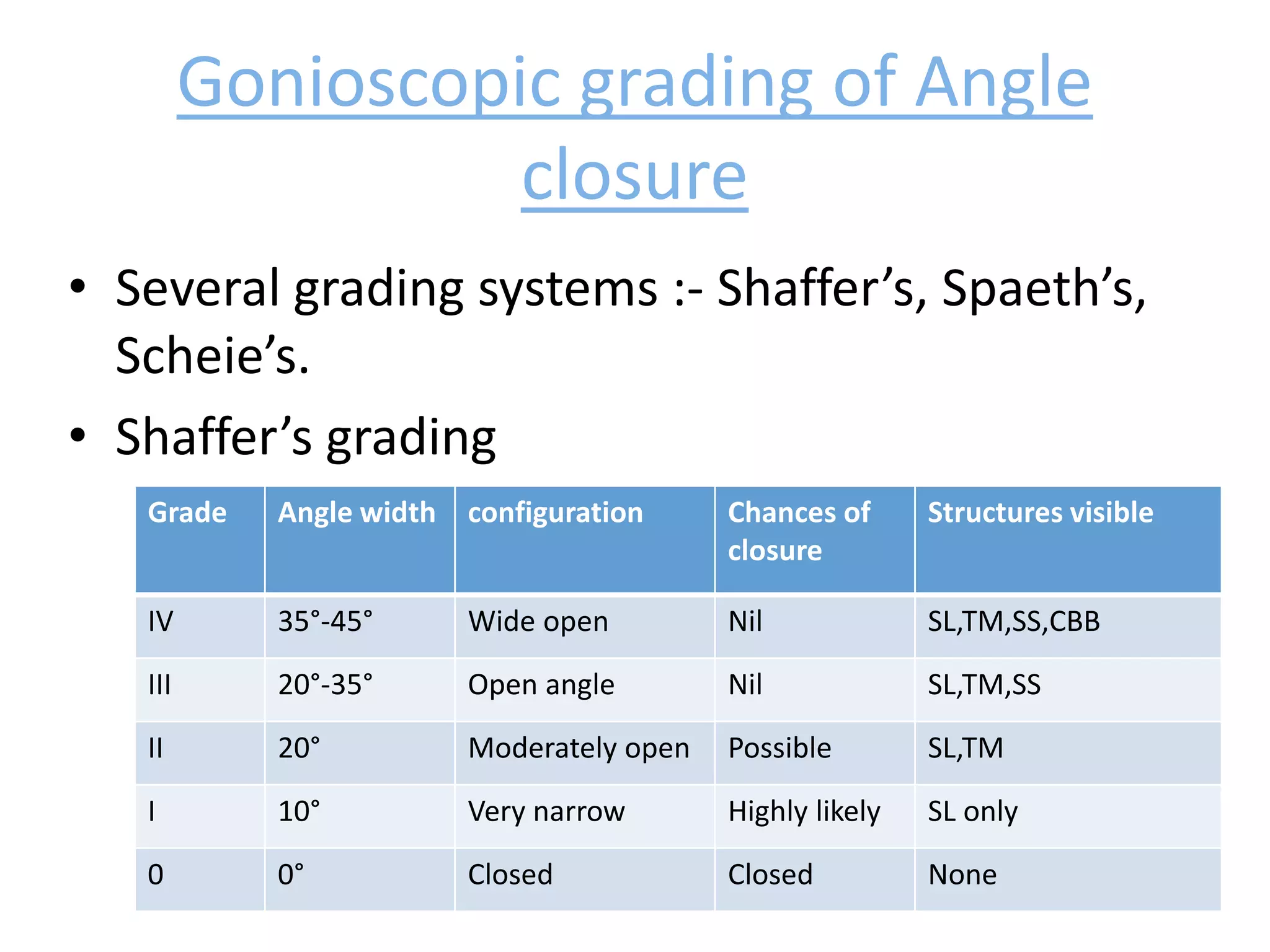
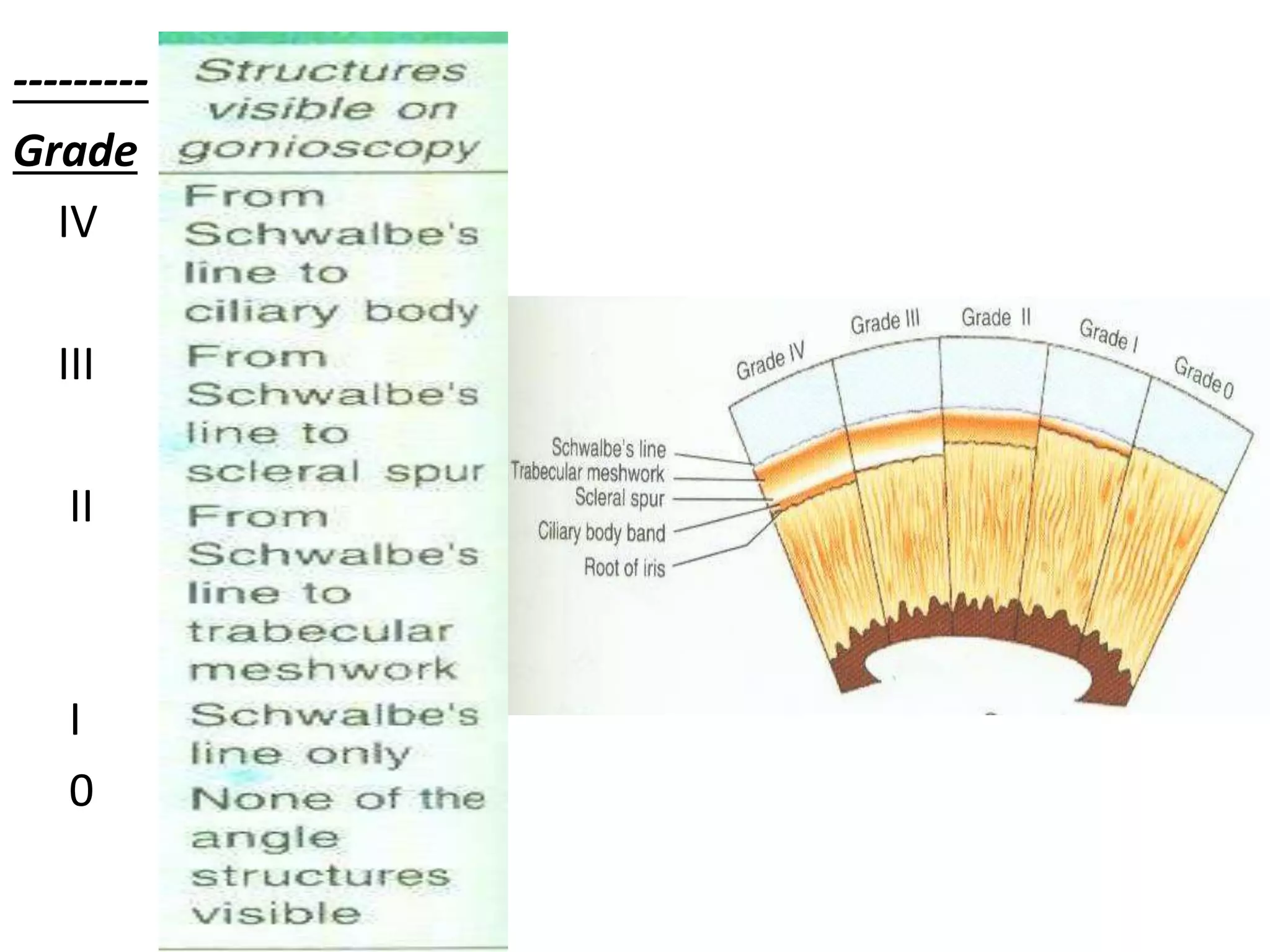
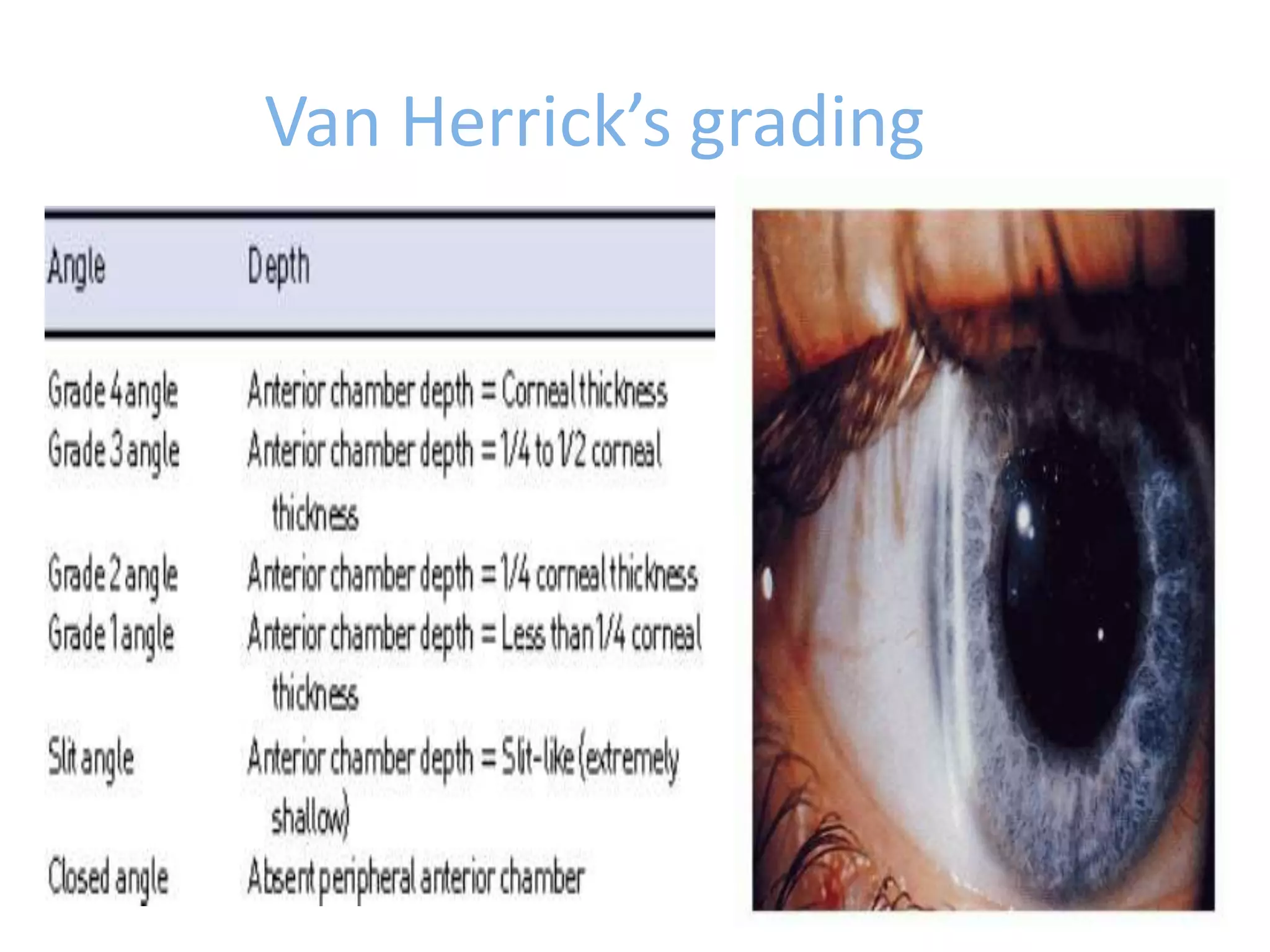
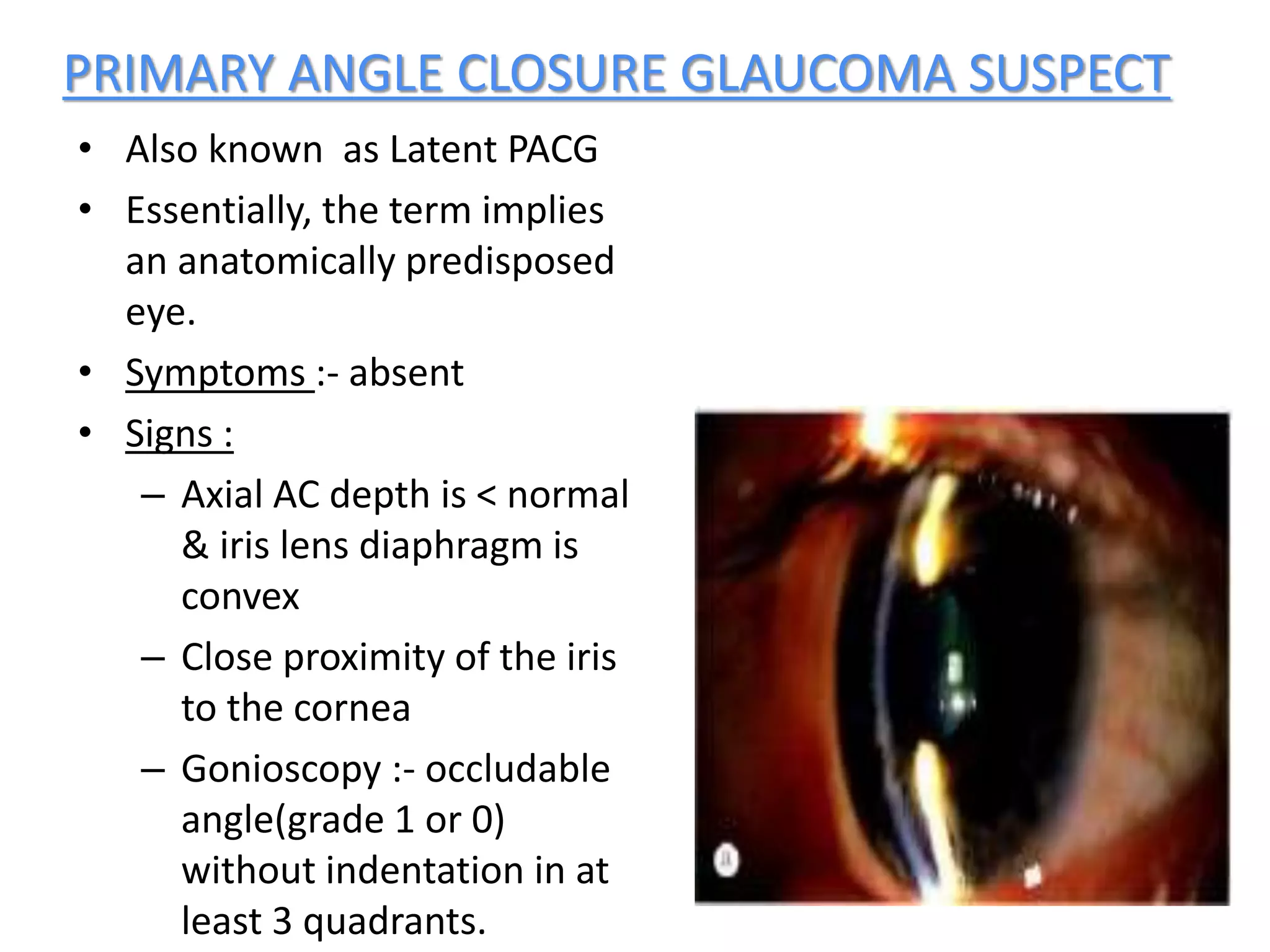
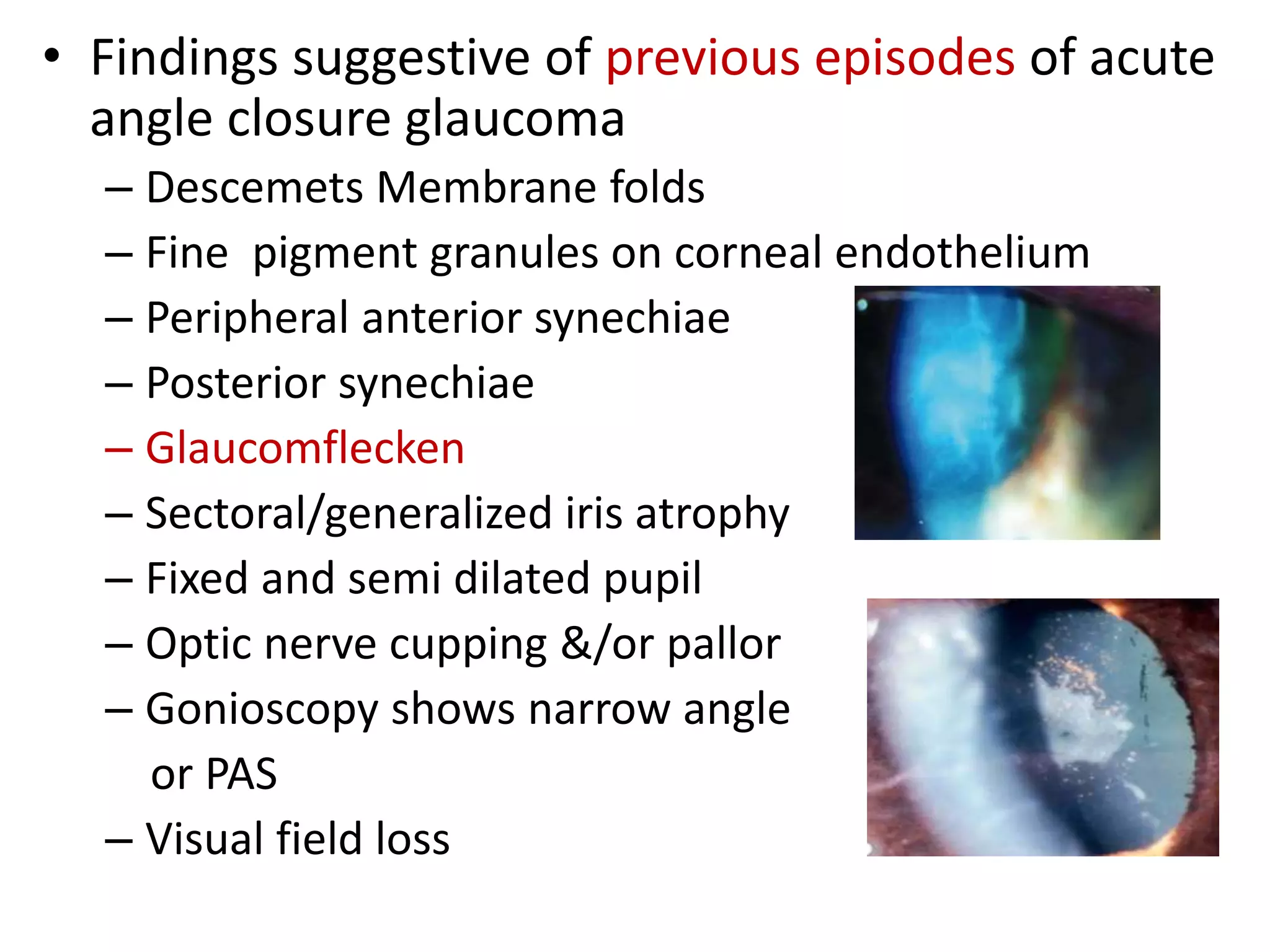
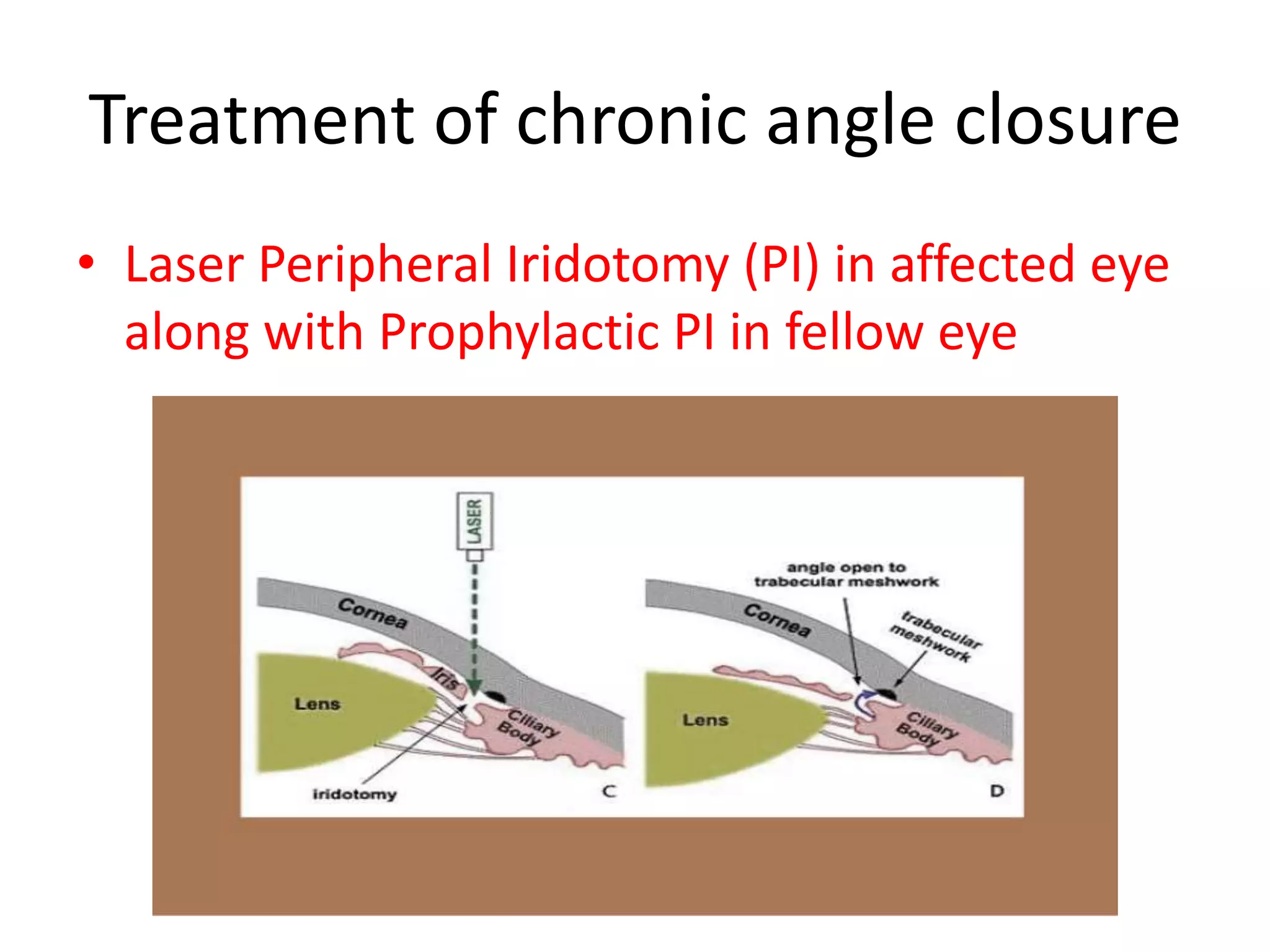
Dr. Ajai Agrawal's presentation defines primary angle closure glaucoma (PACG) as a type of glaucoma characterized by occludable anterior chamber angles that lead to increased intraocular pressure and optic nerve damage. The presentation covers the epidemiology, risk factors, pathogenesis, classification, diagnosis and management of PACG. Treatment may involve medical management, laser peripheral iridotomy to open the angles, or filtering surgeries in advanced cases. Regular follow up is important as PACG can progress to cause vision loss if not properly treated.