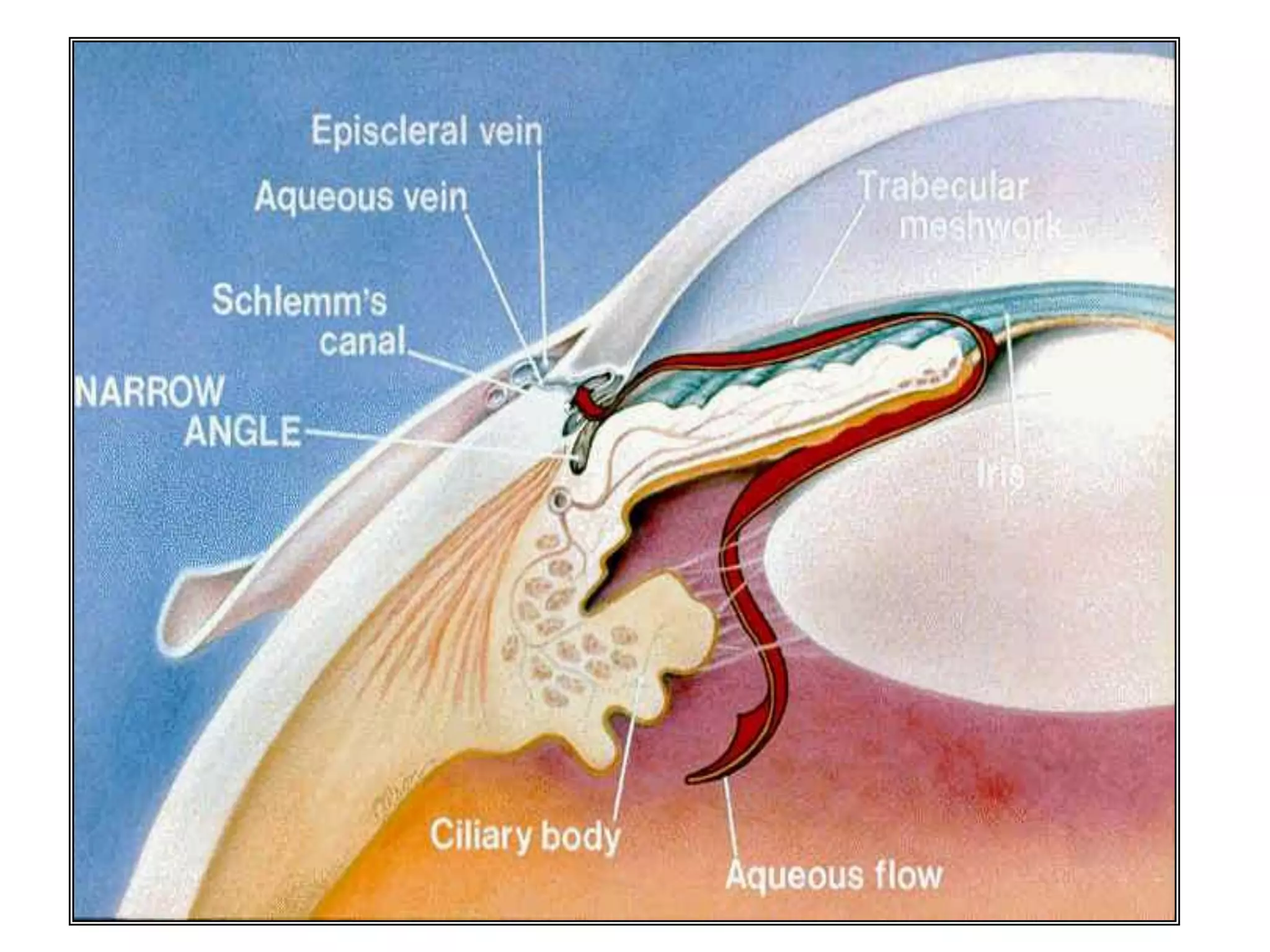
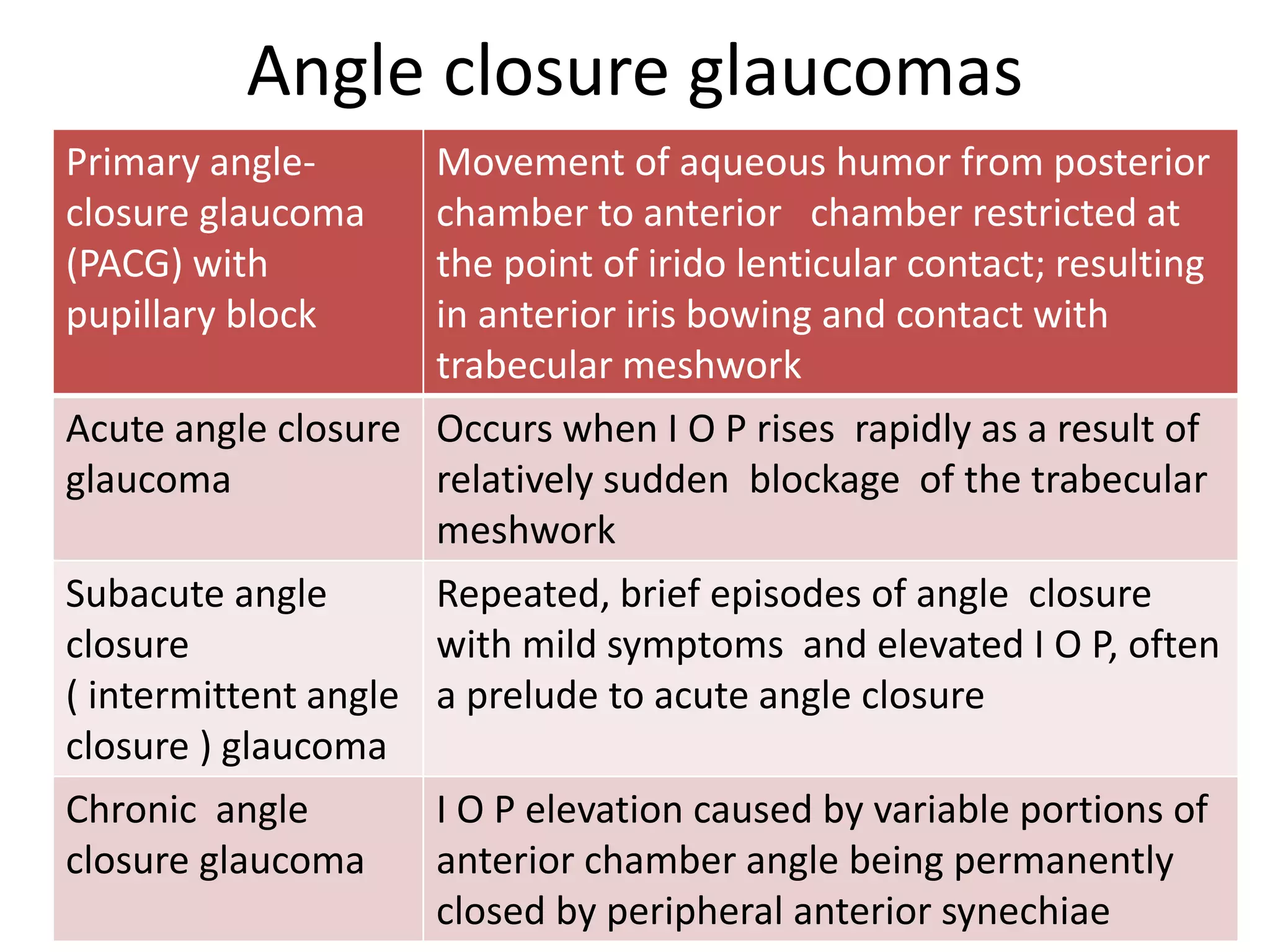
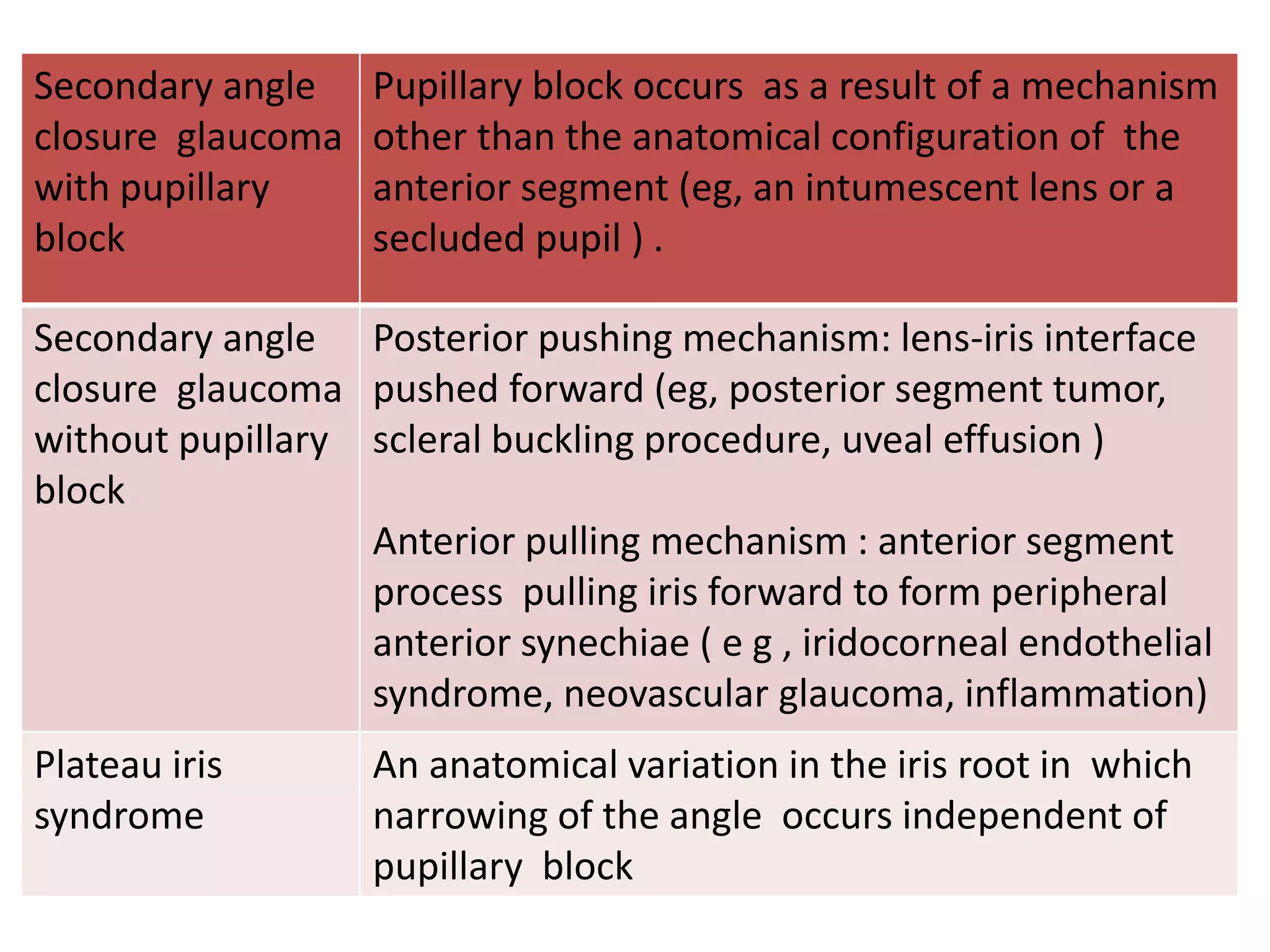
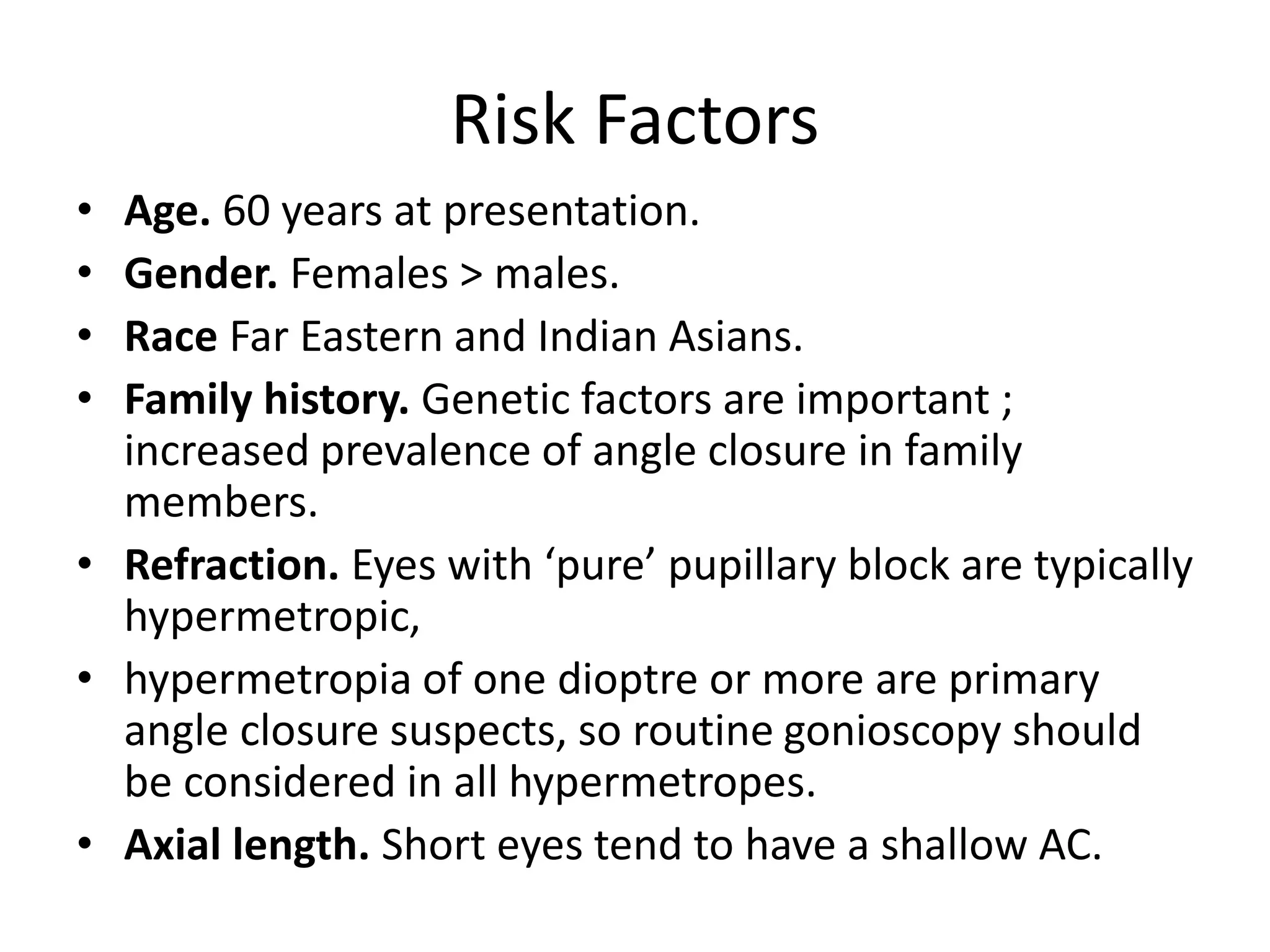
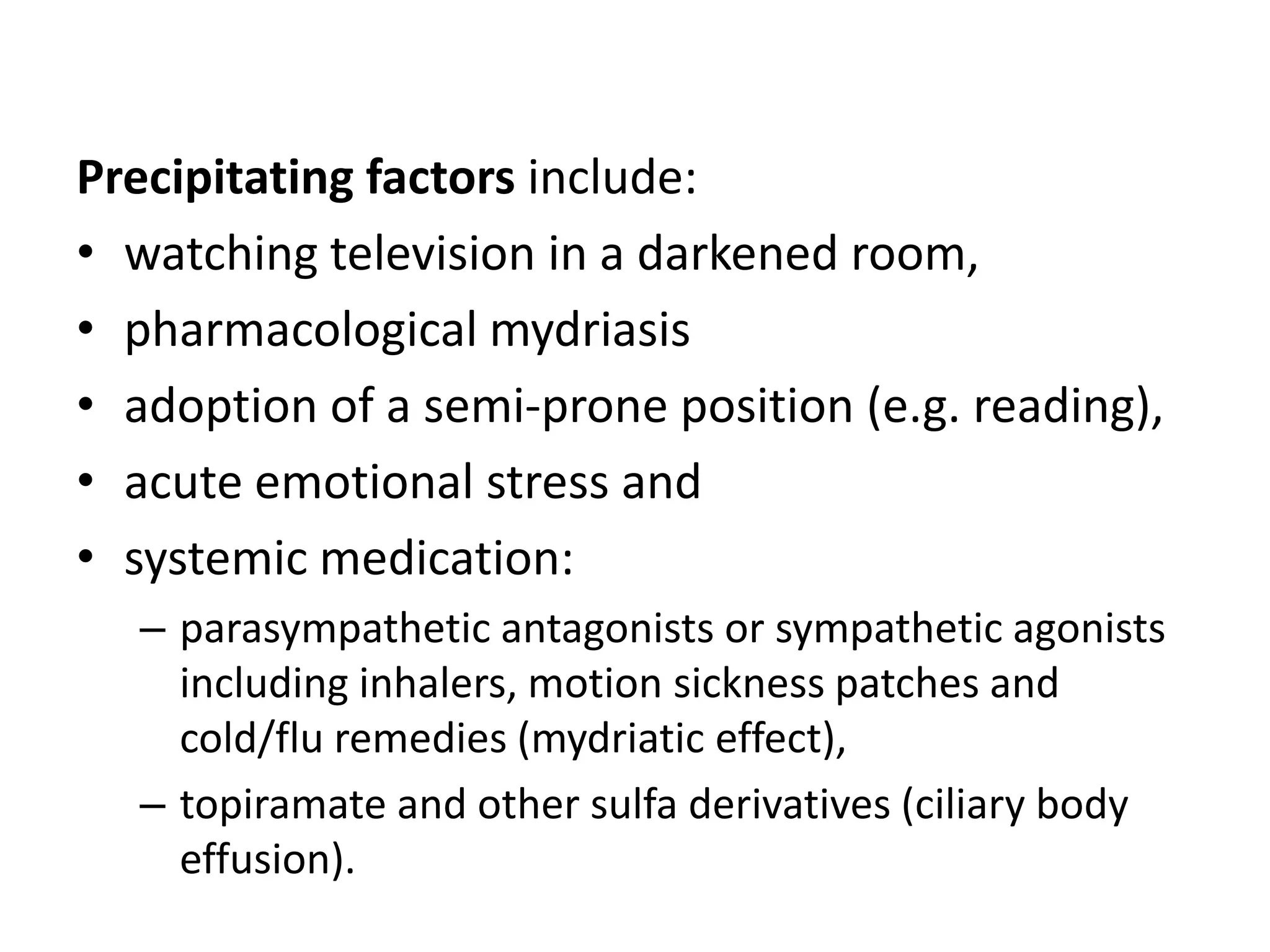
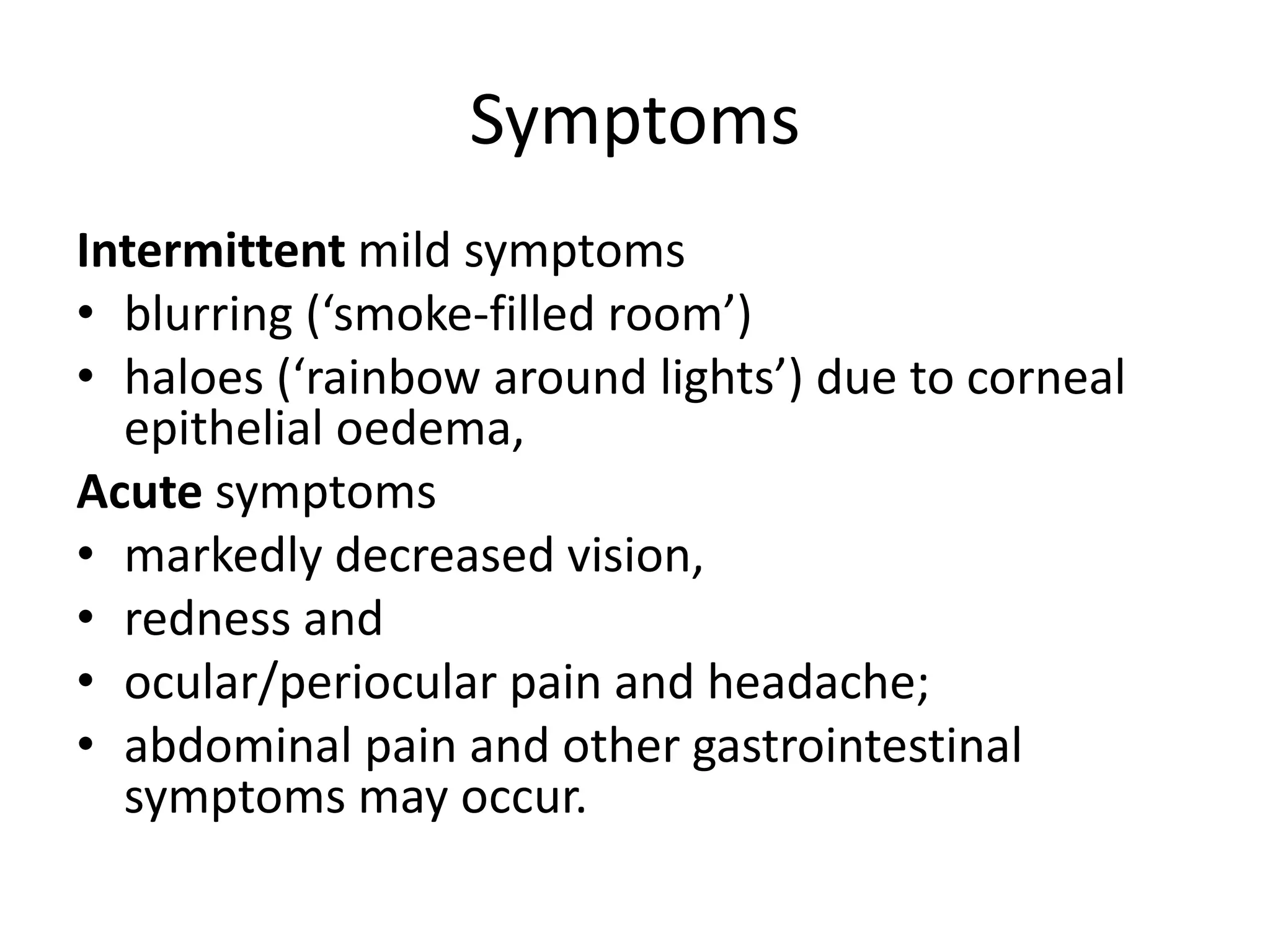
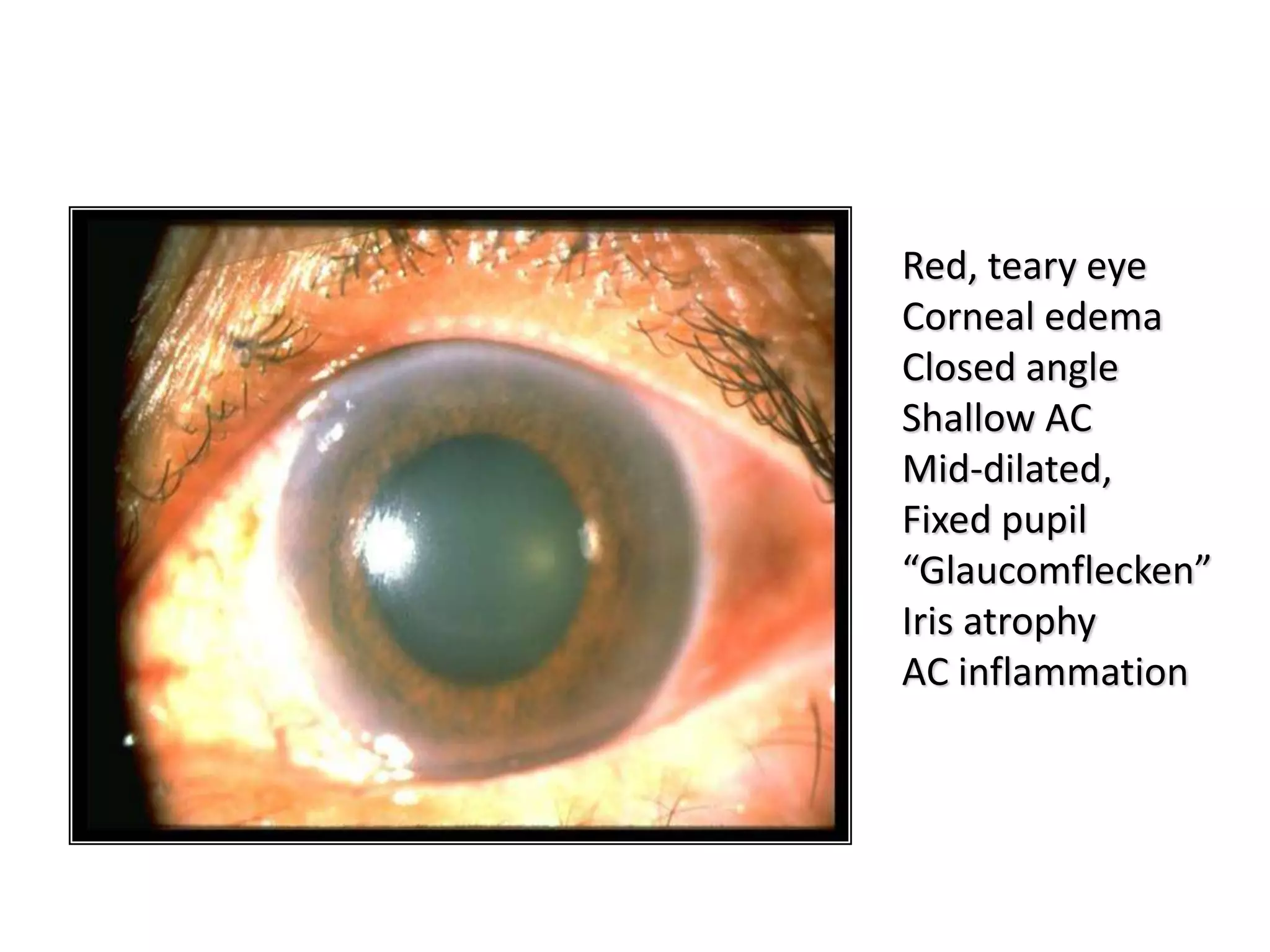
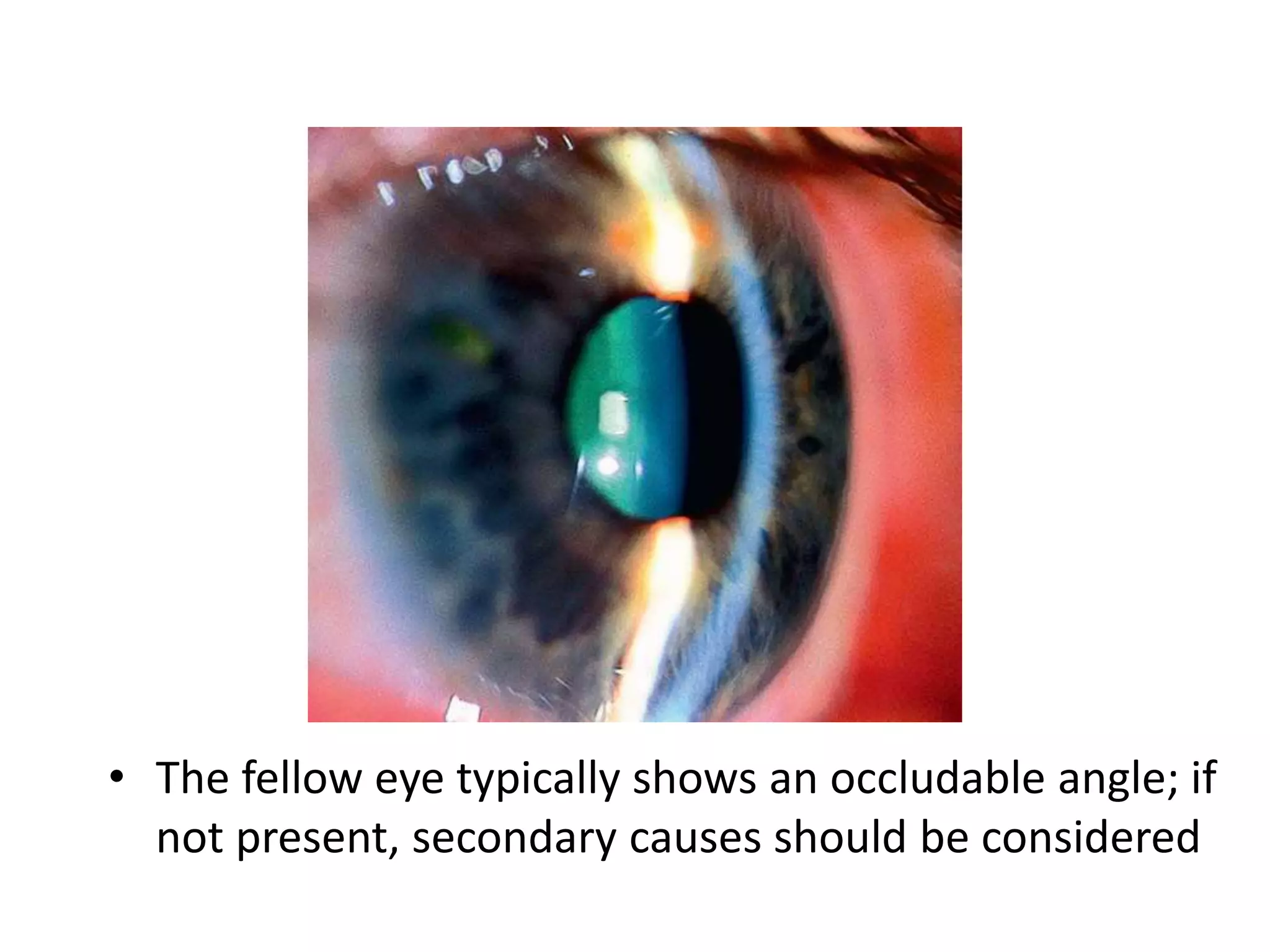
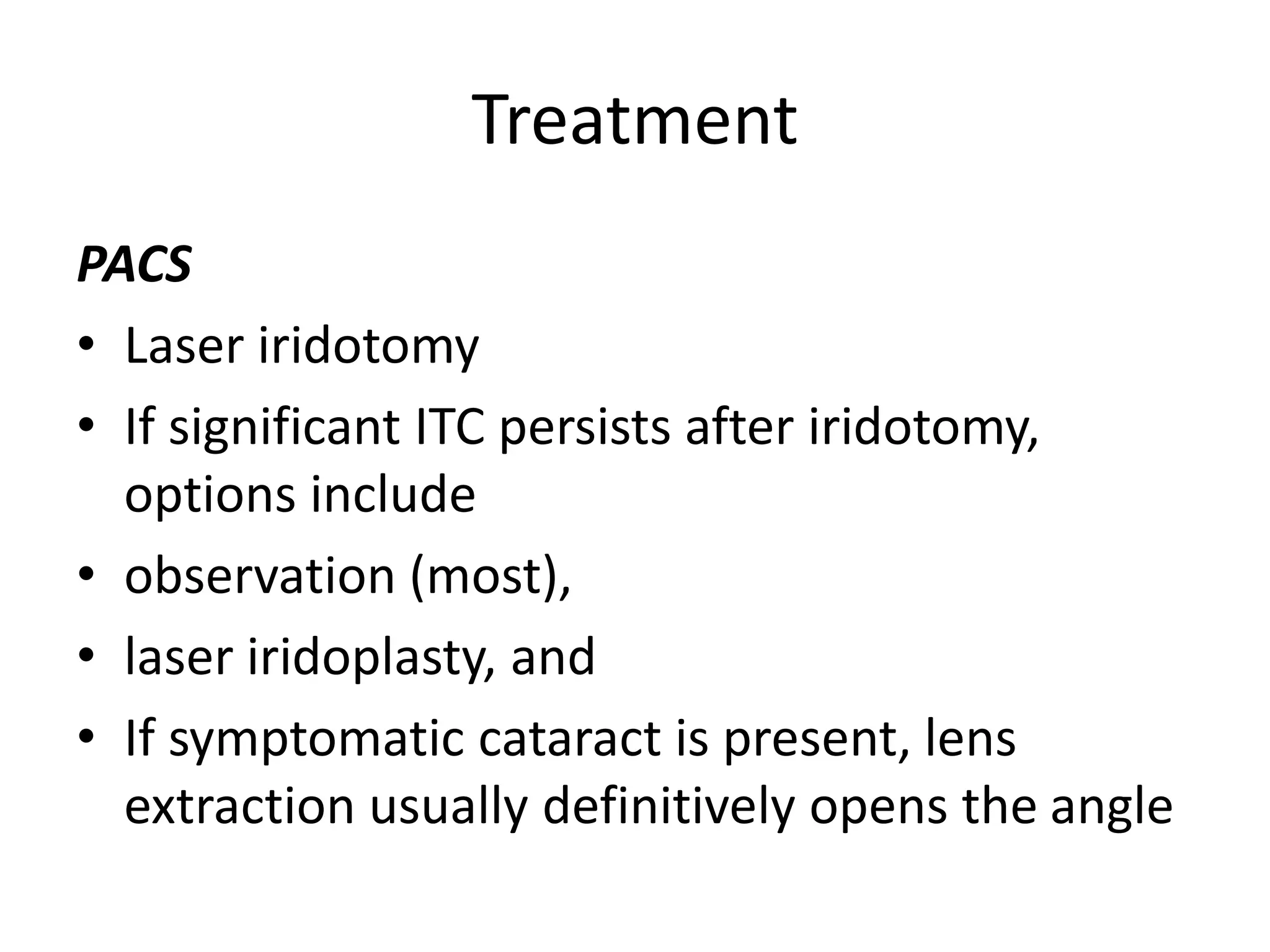
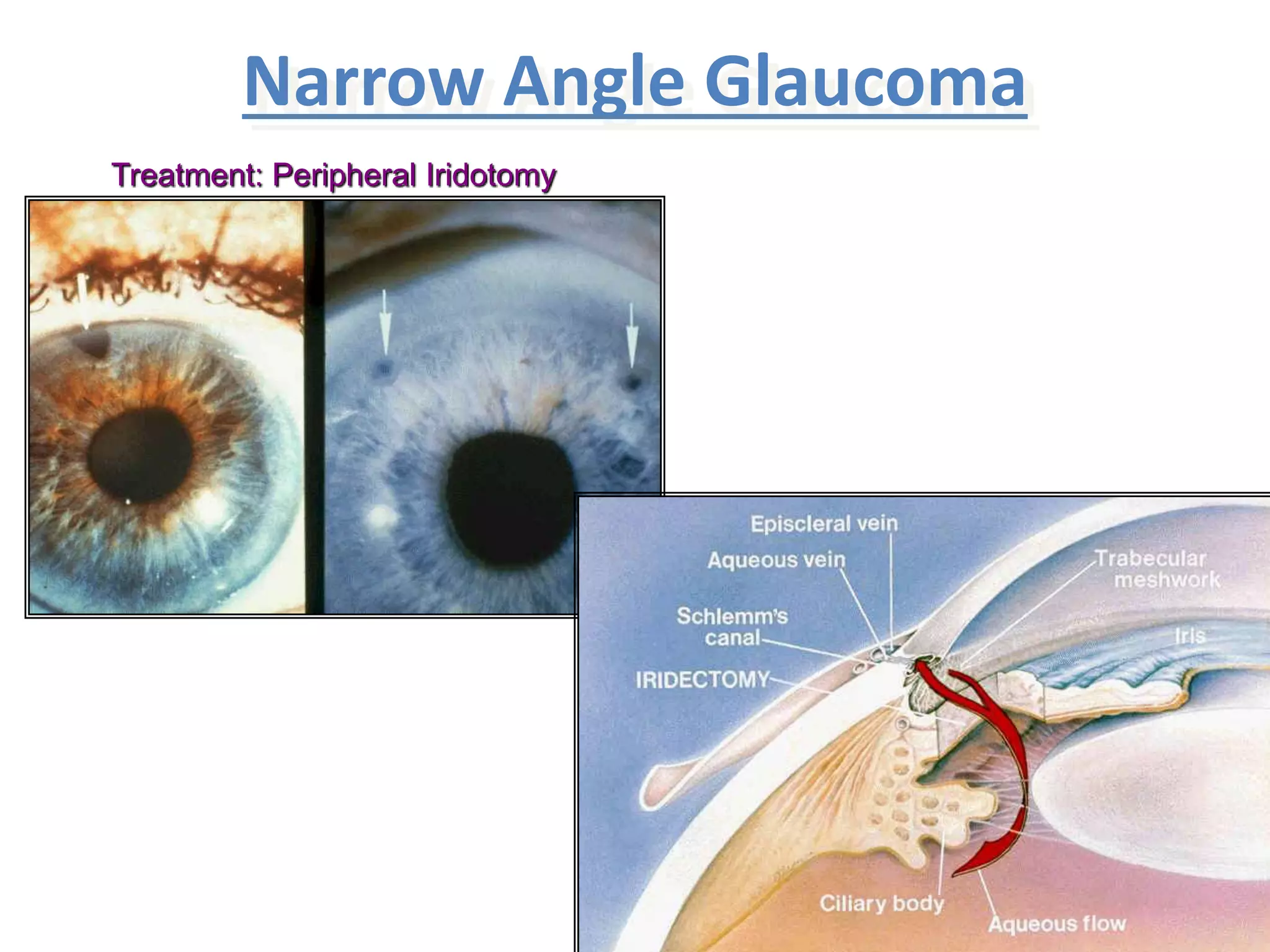
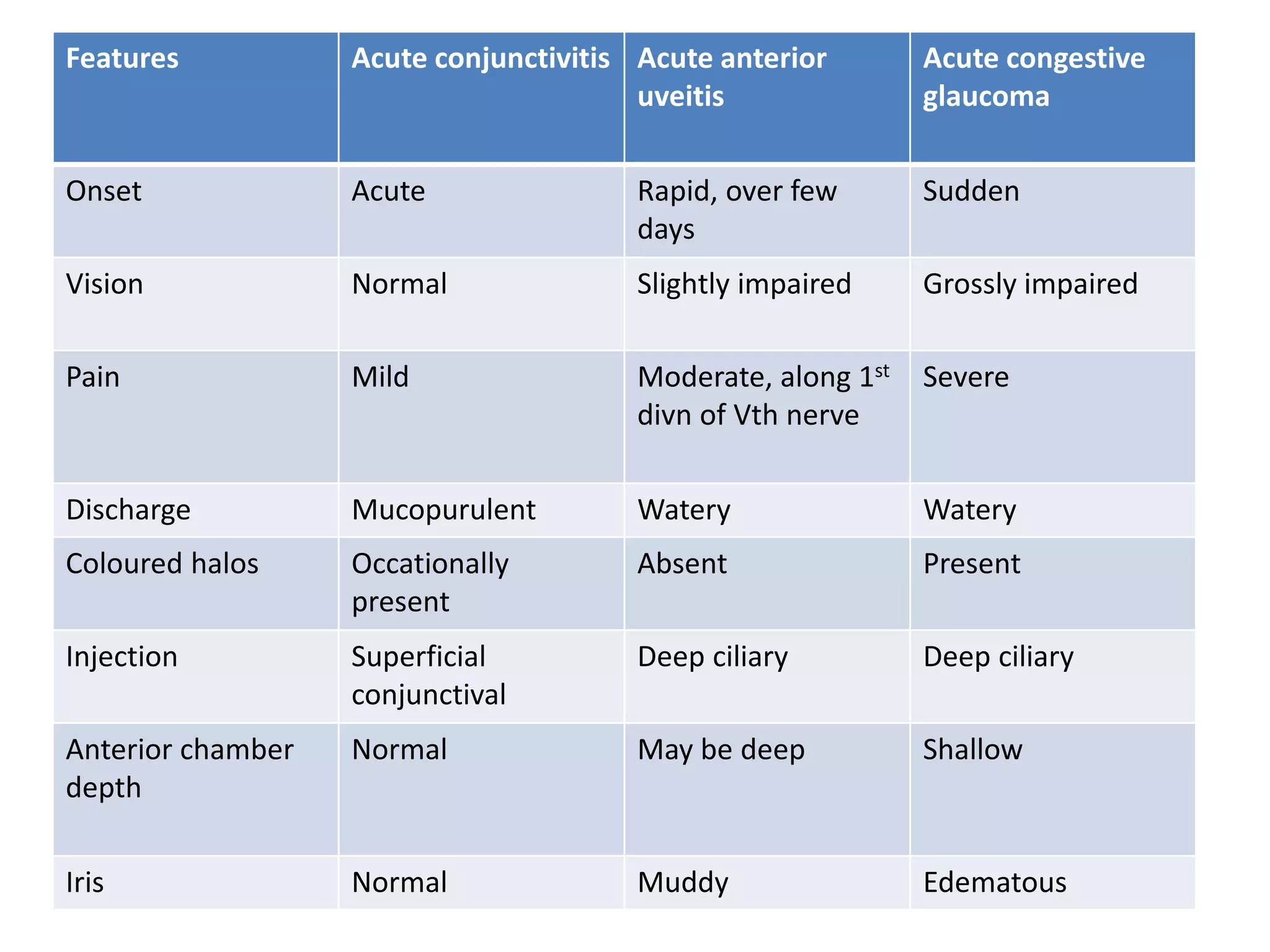
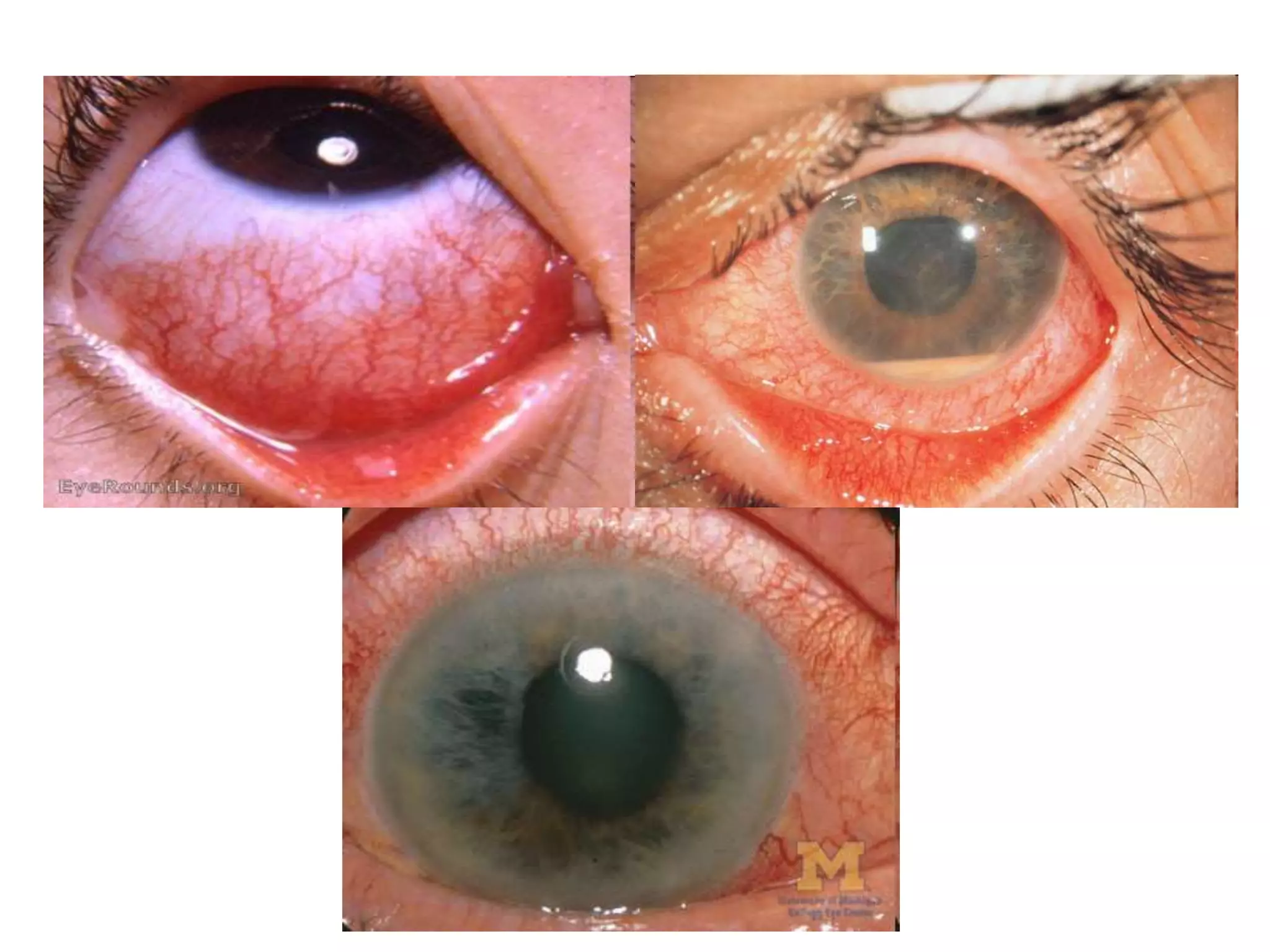
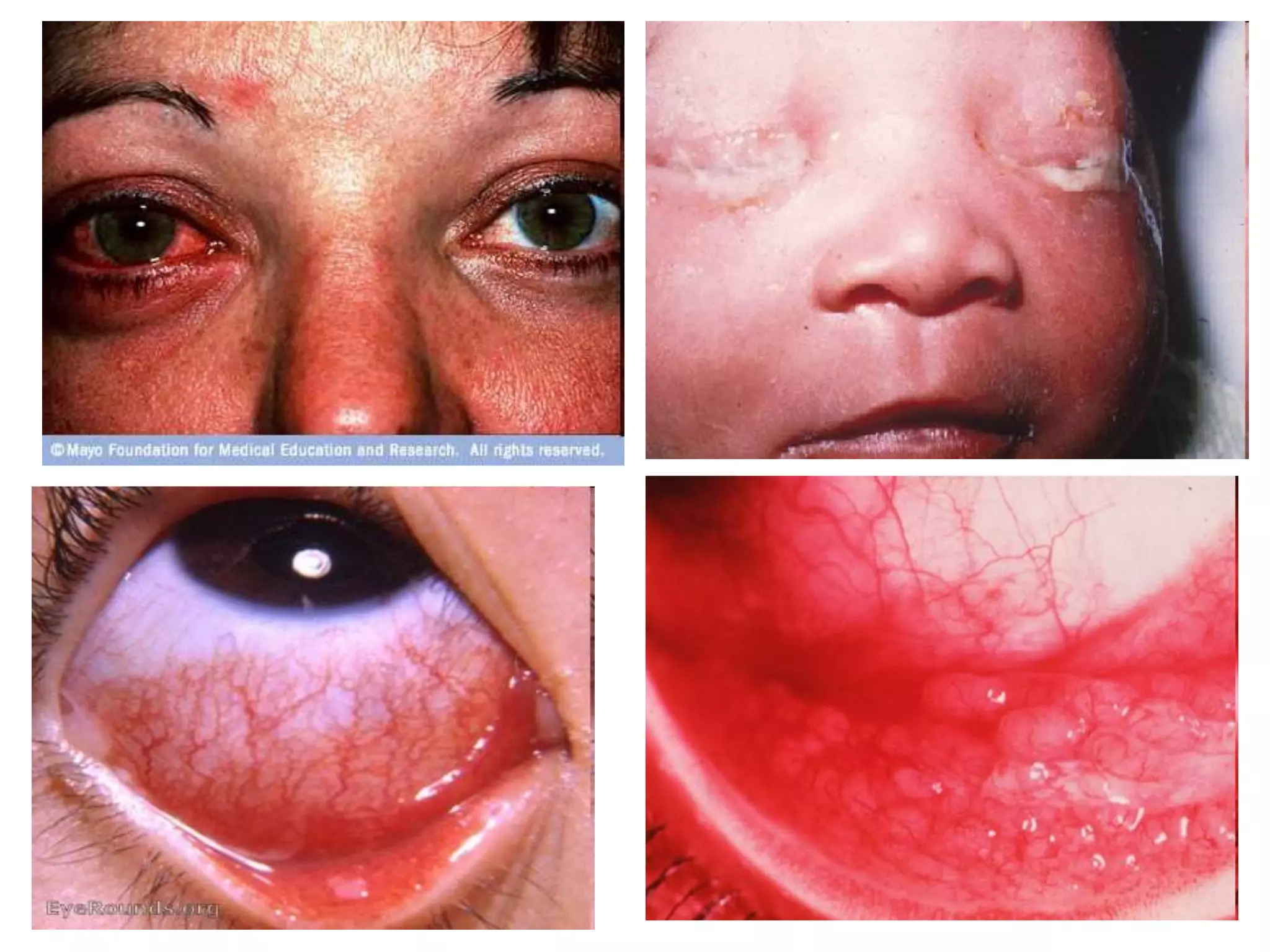
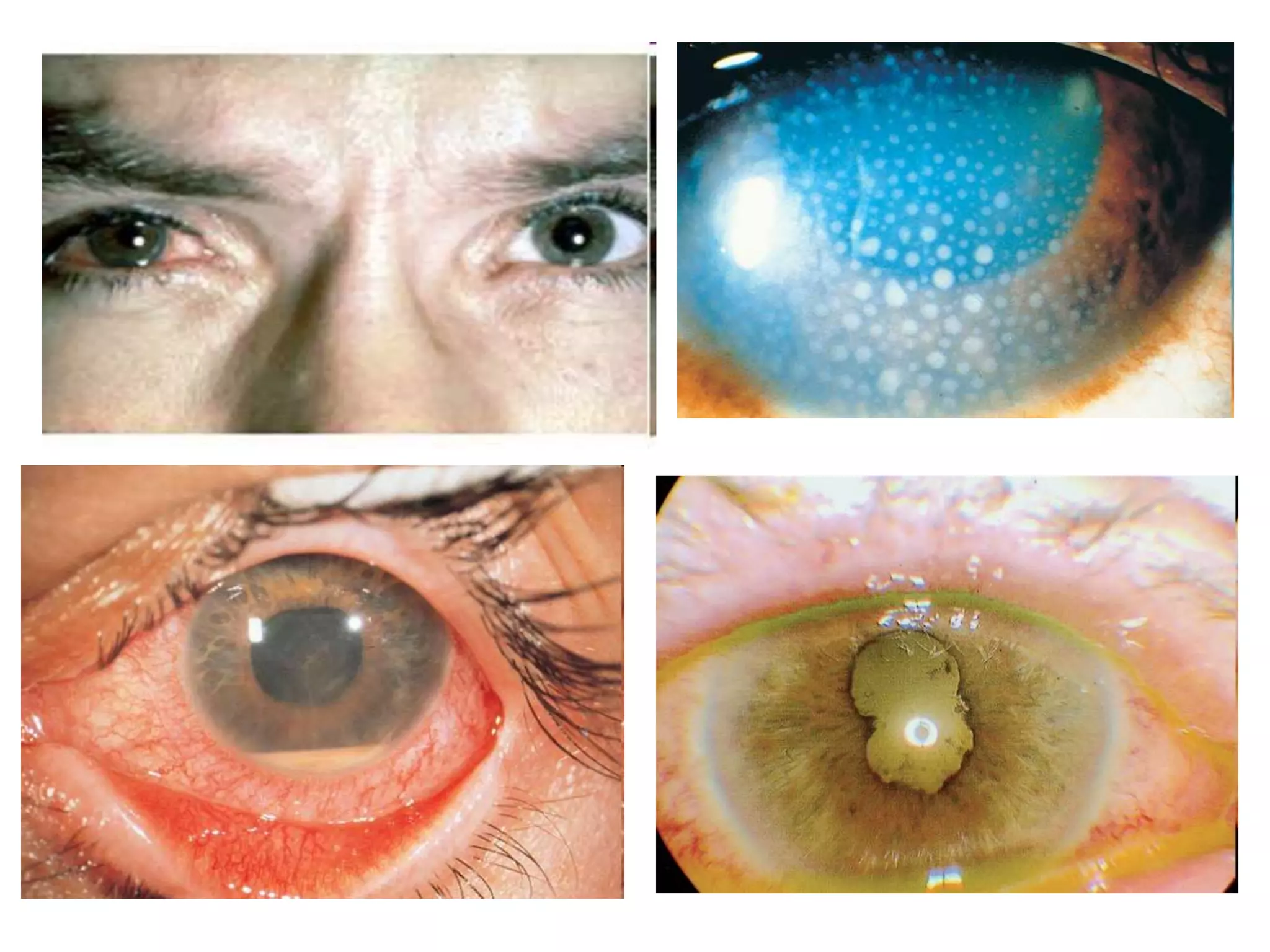
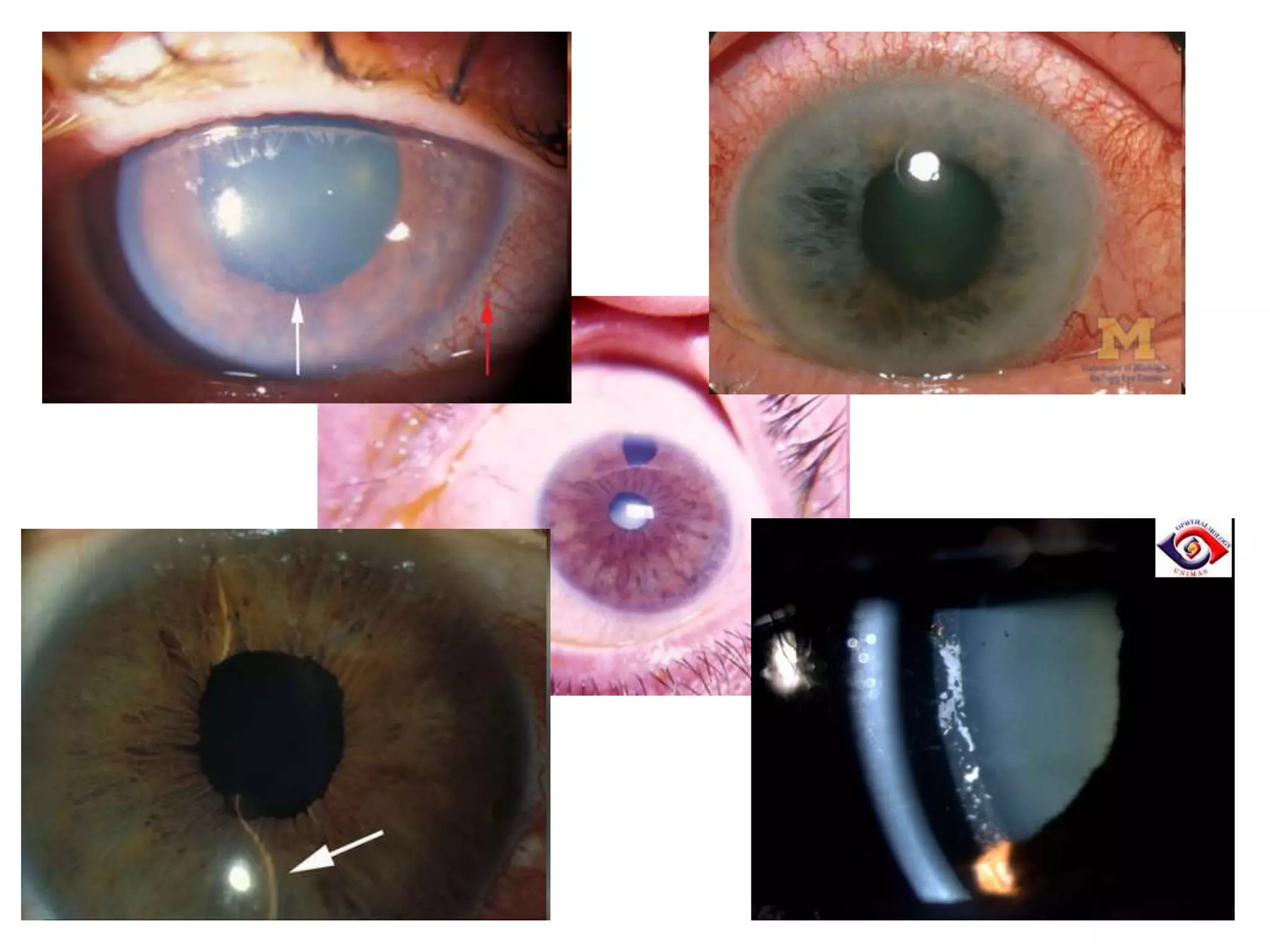
Primary angle closure glaucoma (PACG) involves blockage of the drainage angle between the iris and cornea, increasing intraocular pressure. It has acute, subacute, and chronic stages depending on symptoms and pressure changes. Treatment involves lowering pressure through medications, laser iridotomy to open the angle, or surgery if needed. A red eye from PACG presents with severe vision loss, pain, mid-dilated pupil, and high pressure, distinguishing it from conjunctivitis, uveitis, or other causes.