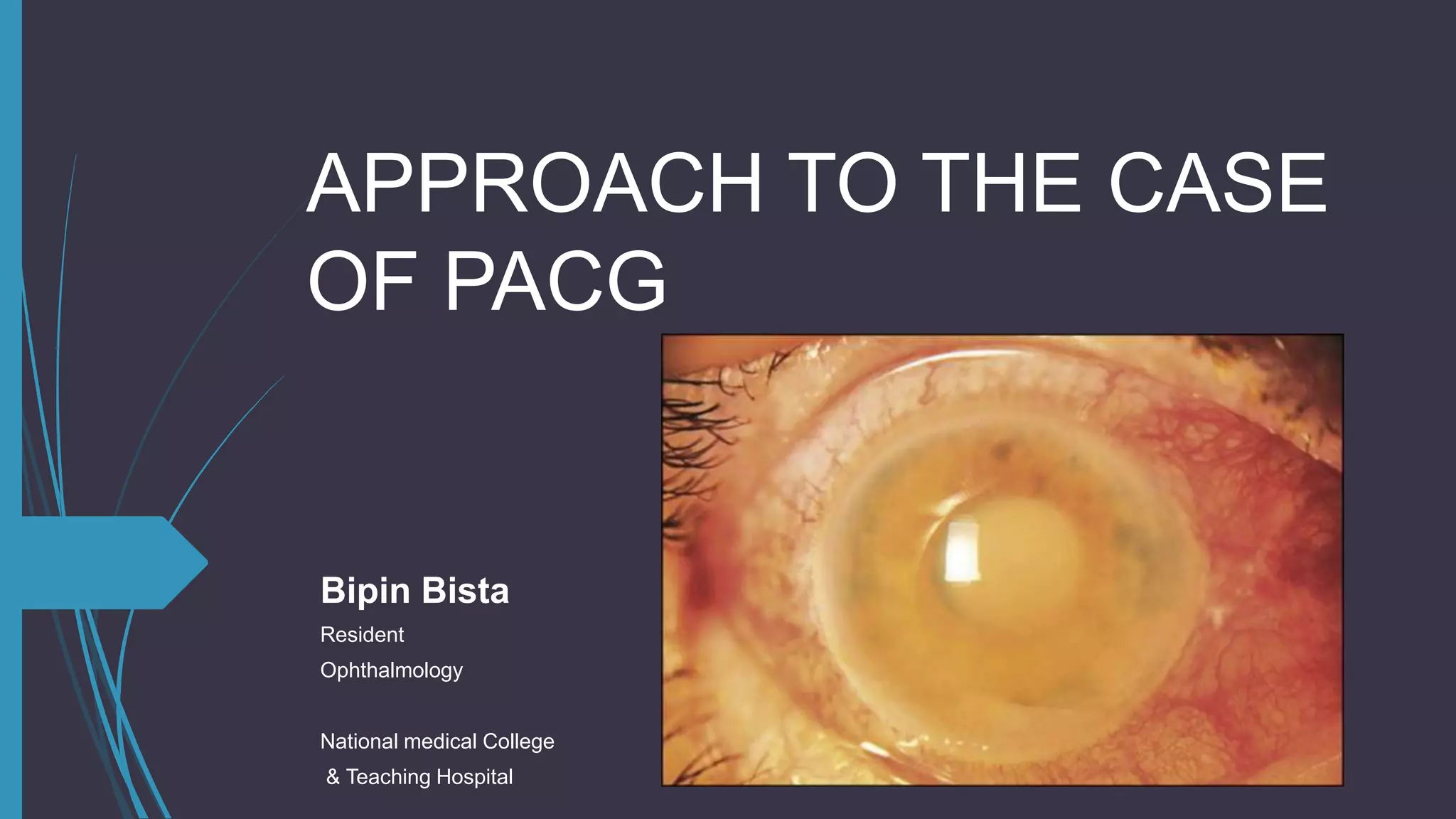
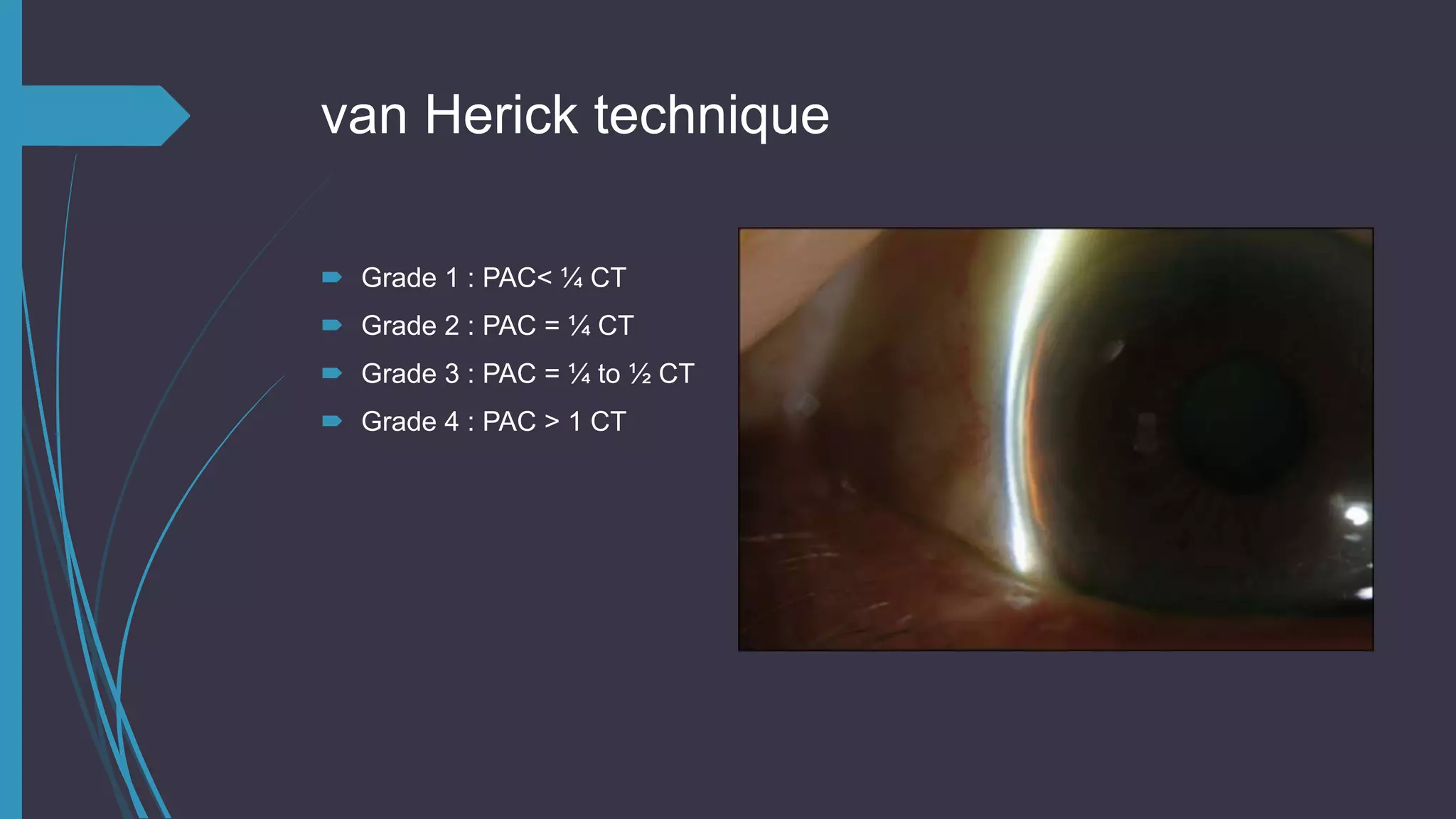
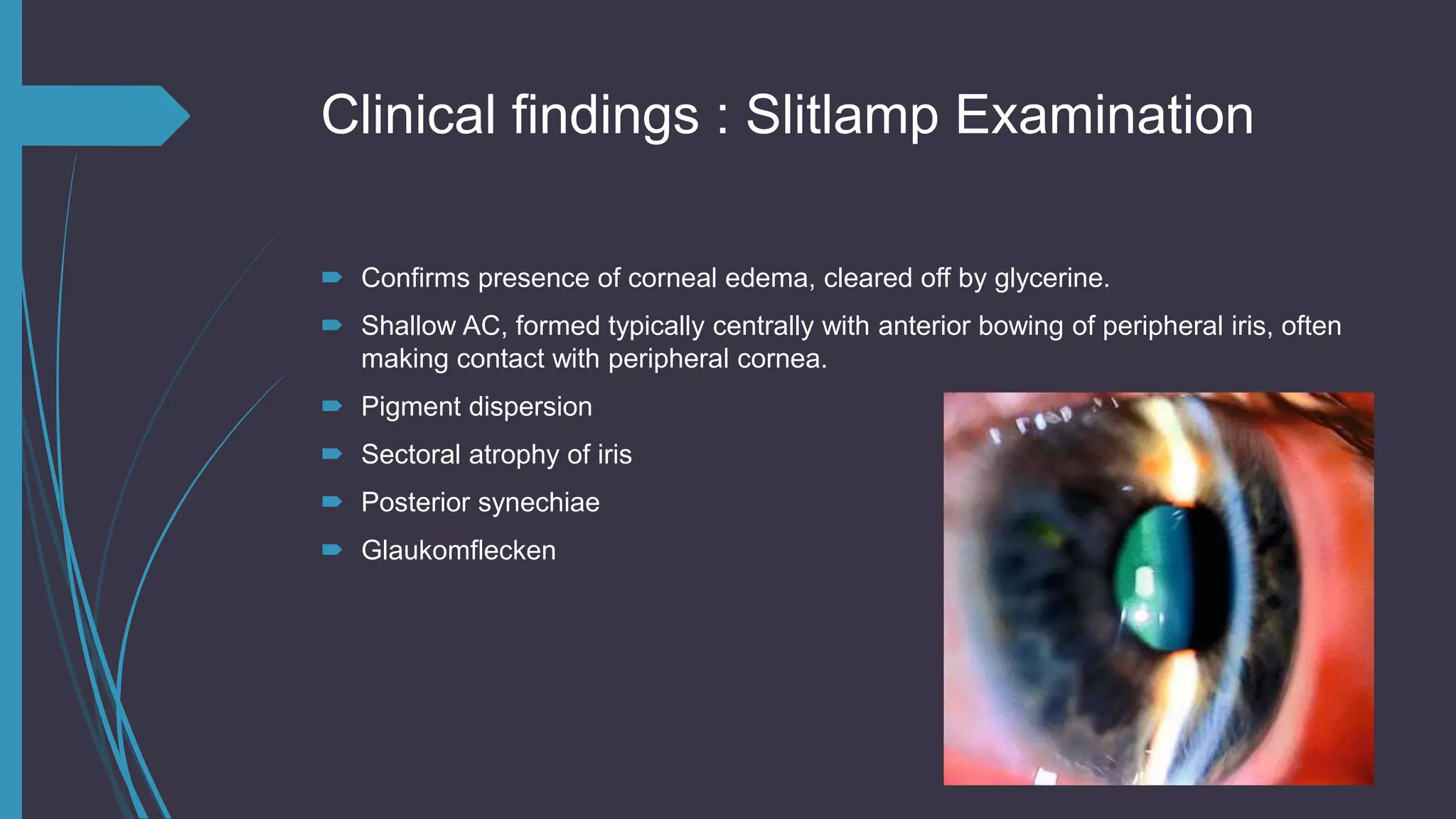
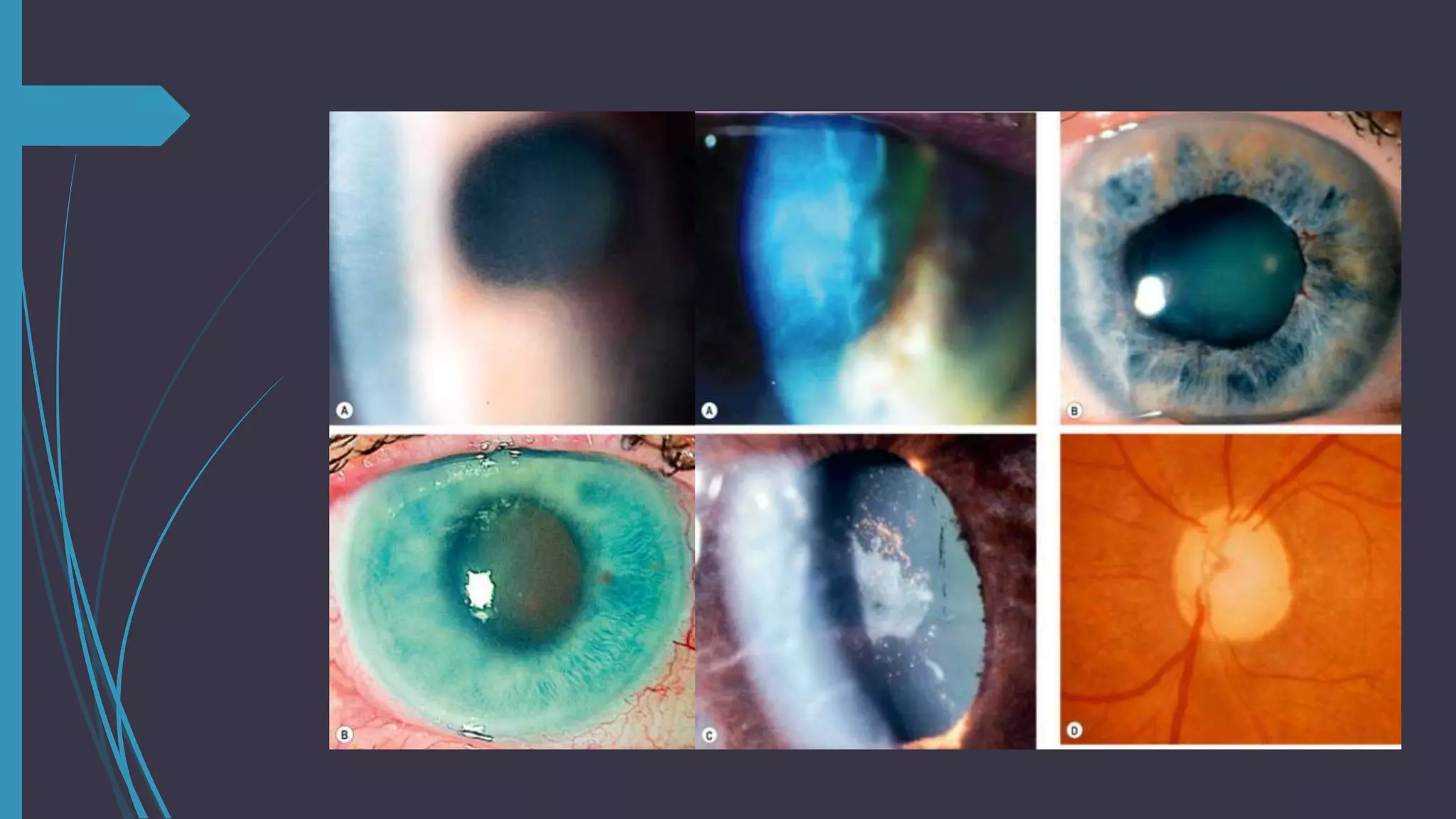
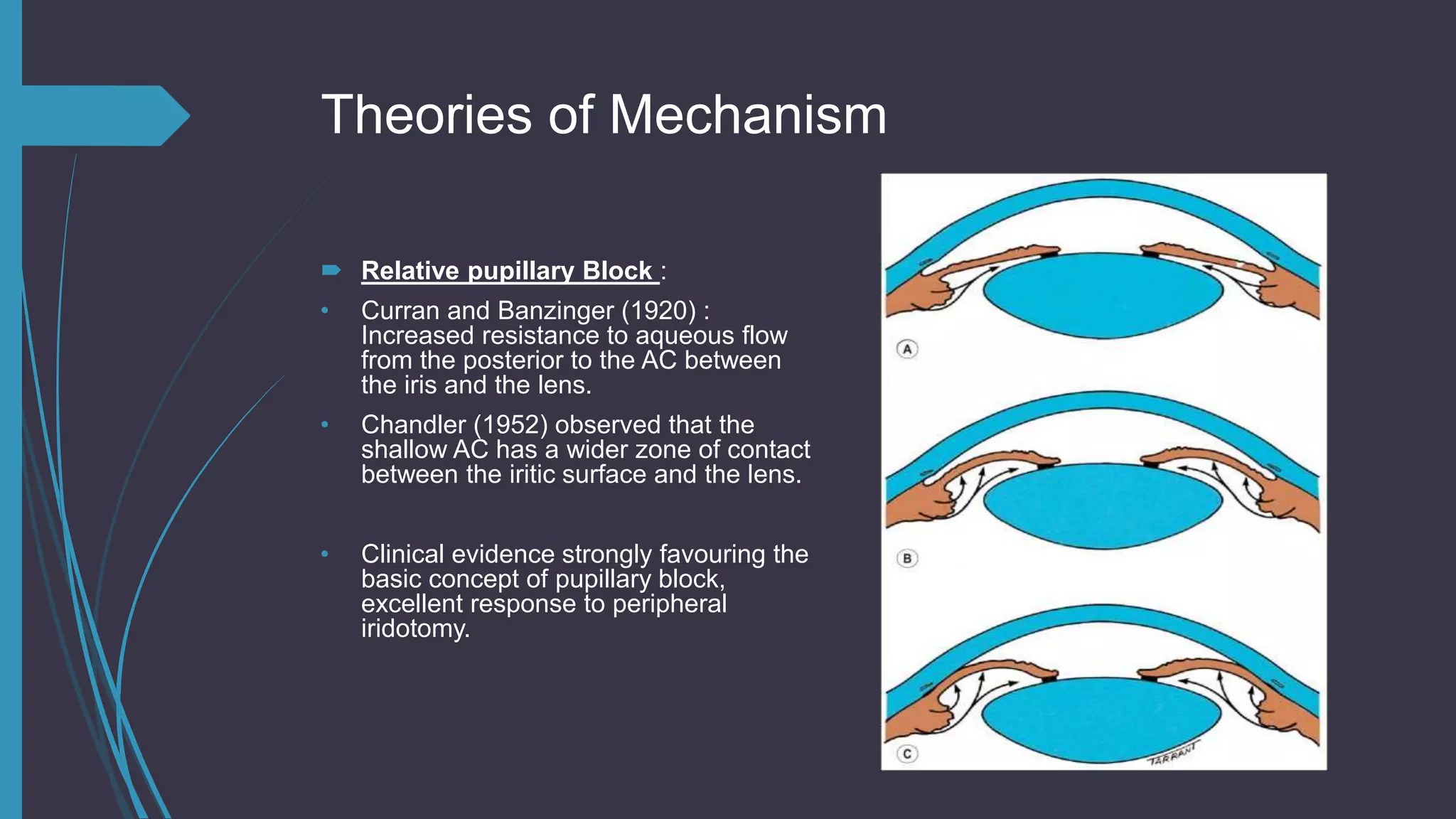
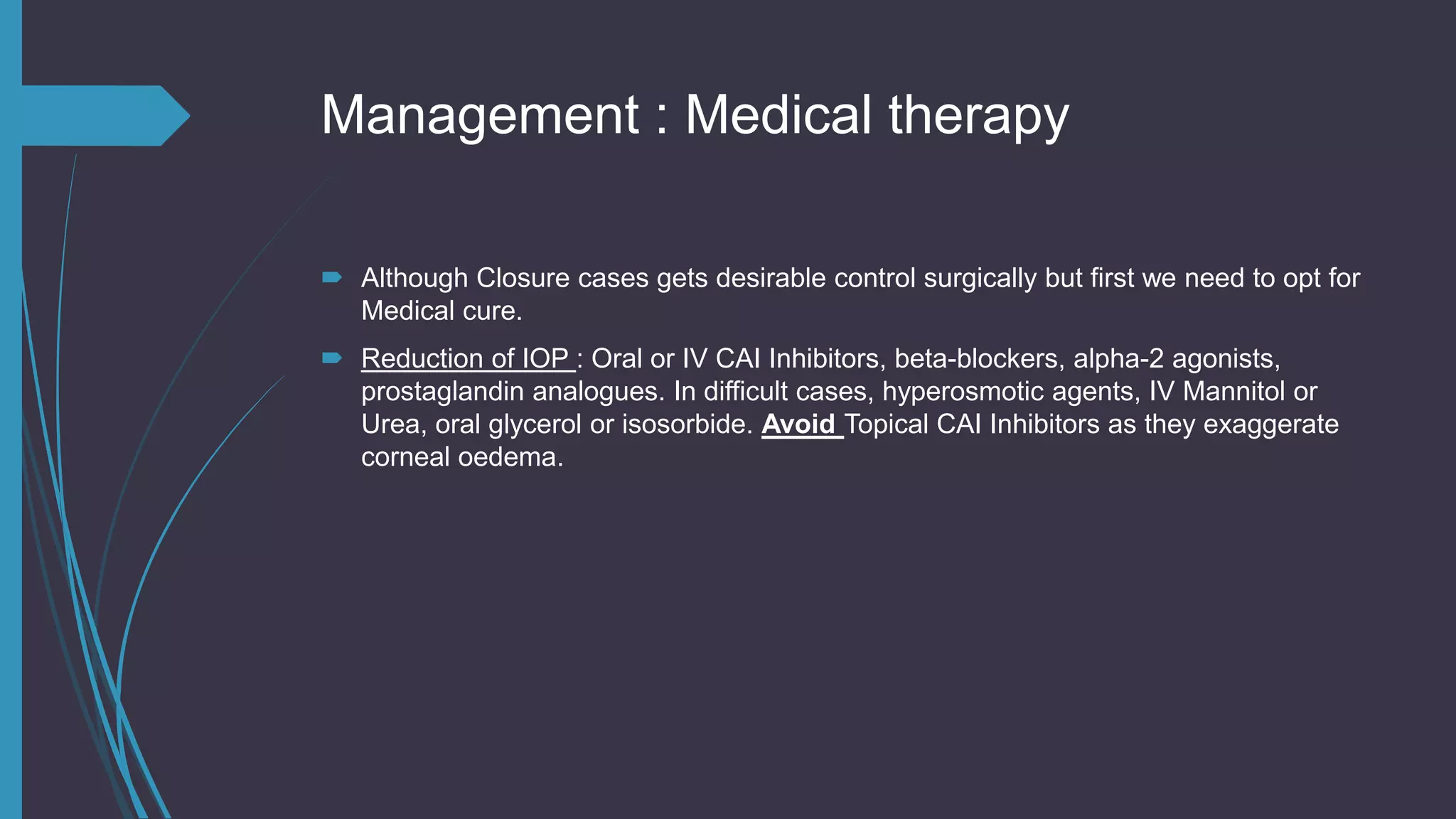
This document provides an overview of the approach to primary angle closure glaucoma (PACG). It begins with definitions and epidemiology, noting it is more common in older females and Asians. Risk factors include age, race, hypermetropia and family history. Examination findings include elevated intraocular pressure, shallow anterior chamber, iris apposition or synechiae on gonioscopy. Symptoms range from acute pain and vision loss to being asymptomatic. Management involves medical therapy to lower pressure initially, followed by laser peripheral iridotomy or filtration surgery depending on the degree of angle closure. The primary mechanism is believed to be pupillary block causing increased resistance to outflow between the iris and lens.