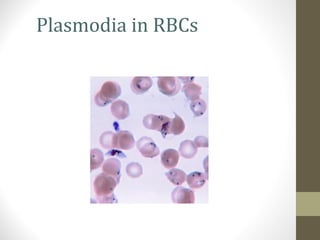
There are over 100 species of Plasmodium, some of which can infect humans and cause malaria. The four main species that infect humans are P. vivax, P. ovale, P. malariae, and P. falciparum. P. falciparum causes the most severe form of malaria and is responsible for over 1 million deaths per year globally. The life cycle of Plasmodium involves both sexual and asexual reproduction in humans and mosquitoes. Female Anopheles mosquitoes transmit the parasite between humans during blood-feeding. Laboratory diagnosis of malaria is usually done by examining thick and thin blood smears under a microscope to look for the parasite in red blood cells. Treatment depends on the species,