This document summarizes information about malaria, including:
1) Malaria is caused by protozoan parasites of the genus Plasmodium, with four species infecting humans. P. falciparum causes the most severe disease.
2) Malaria is transmitted by the bite of infected female Anopheles mosquitoes. The parasite has a complex life cycle alternating between human and mosquito hosts.
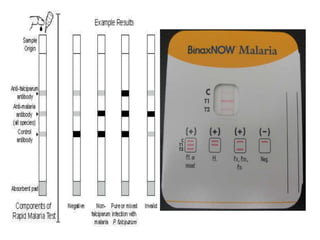
3) Symptoms vary depending on the Plasmodium species, but microscopically parasites can be seen in red blood cells on blood smears. Rapid diagnostic tests also detect parasite antigens.


























![WHO definition and Classification of Drug
Resistance
Ability of a parasite to multiply or to survive in the presence of
concentrations of a drug that normally destroy parasites of the
same species or prevent their multiplication.
Three levels of resistance[R] are defined by WHO
RI: following treatment, Parasitaemia clears but a recrudescence
occurs
RII: following treatment, there is a reduction but not a clearance
of parasitaemia
RIII: Following treatment, there is no reduction of parasitaemia
Method classifying resistance, based on counting trophozoites
in blood films for upto 7 days after treatment and monitoring
the patient for any subsequent recrudescence](https://image.slidesharecdn.com/malarialabdiagnosis-210623100846/85/Malaria-lab-diagnosis-30-320.jpg)

