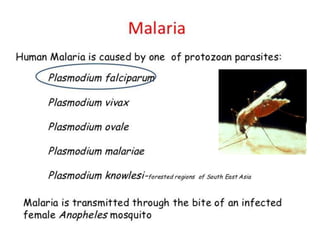
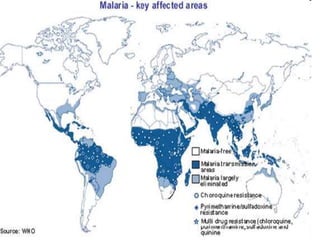
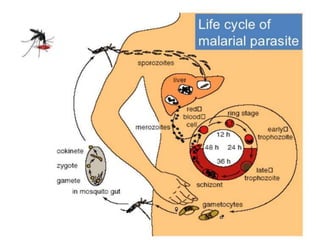
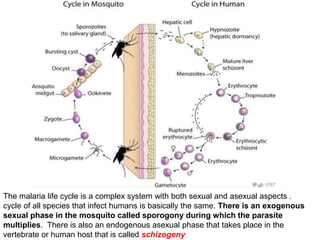
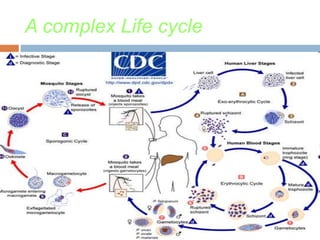
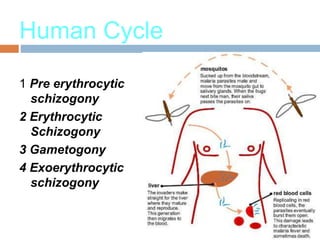
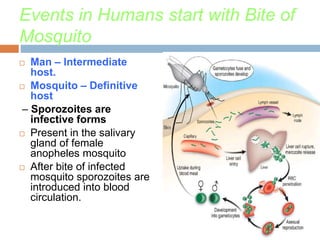
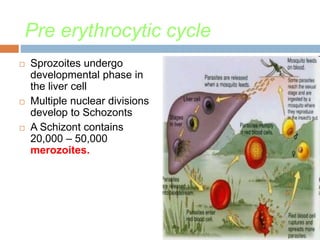
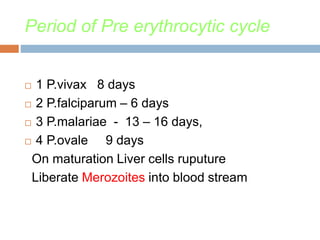
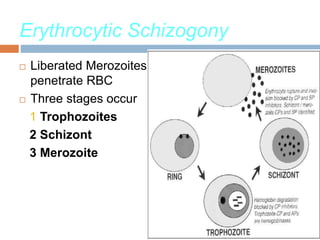
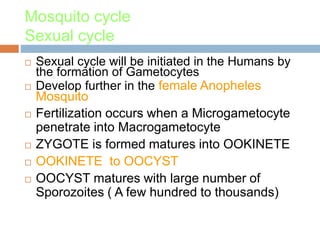
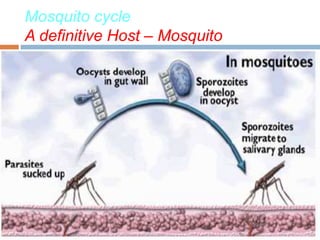
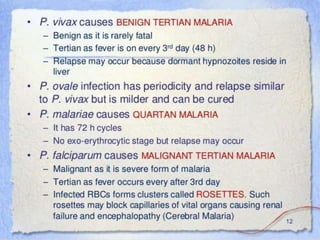
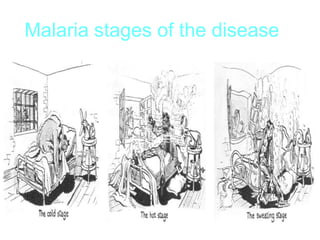
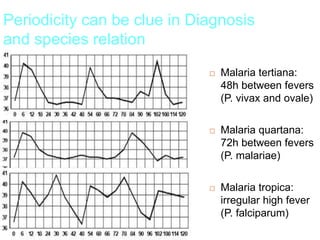
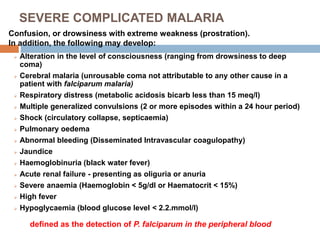
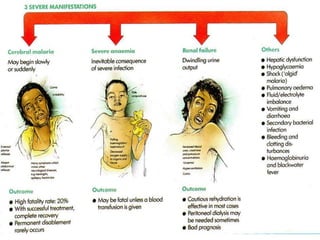
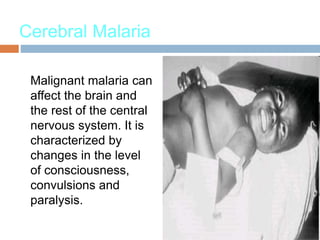
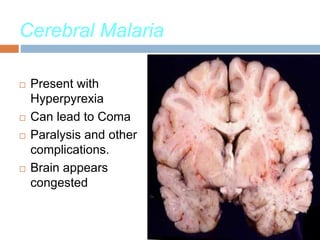
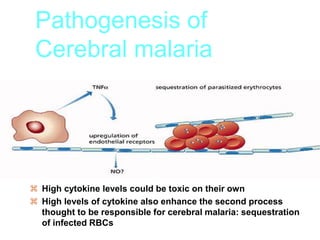
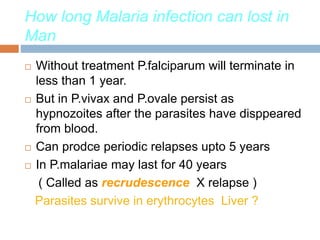
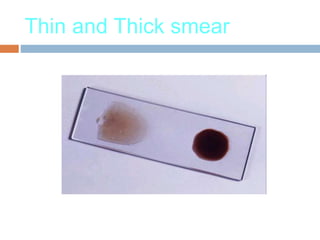
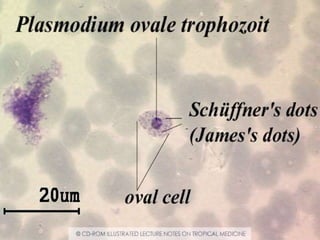
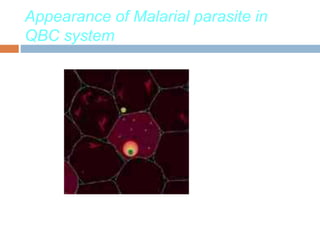
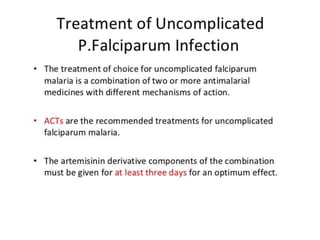
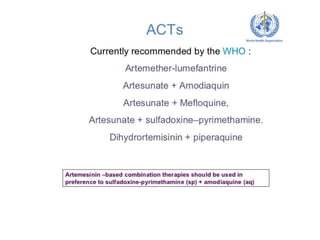
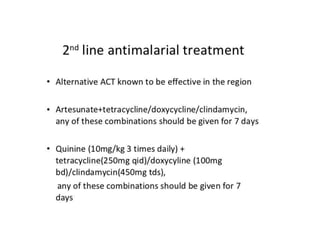
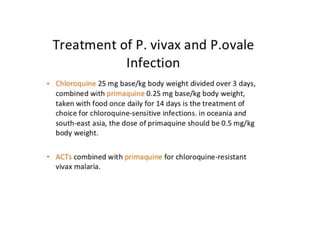
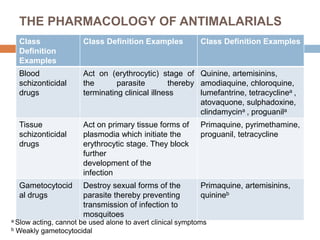
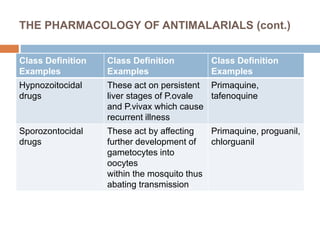
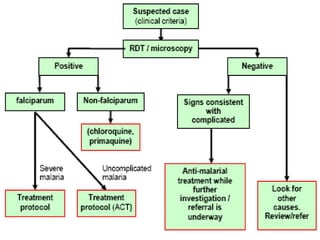
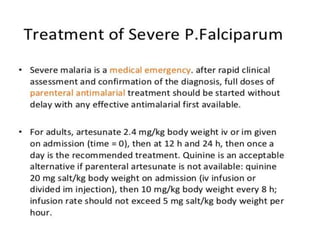
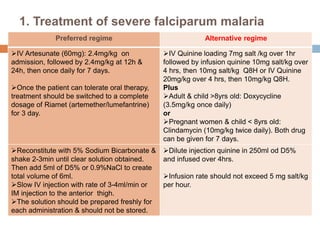
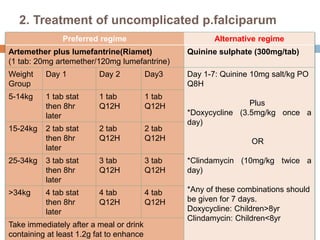
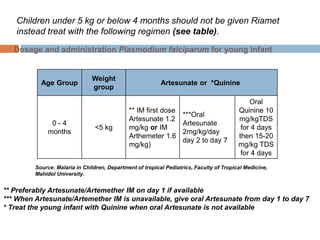
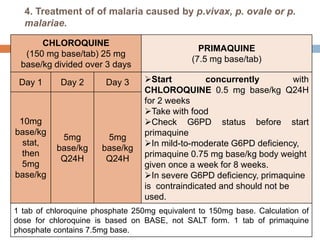
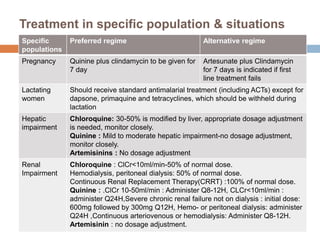
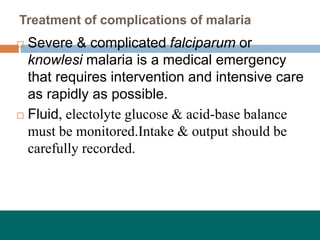
Malaria remains a devastating global health issue, infecting hundreds of millions annually. It is caused by Plasmodium parasites and transmitted via Anopheles mosquitoes. The malaria lifecycle involves both asexual and sexual reproduction in the human and mosquito hosts. In humans, the parasites multiply in the liver and infect red blood cells, causing symptoms like fever, chills, and headaches in cycles. Untreated, P. falciparum malaria can cause severe complications like cerebral malaria. Diagnosis involves examining blood films microscopically or using rapid tests to detect parasites or antigens. While some drugs like chloroquine once treated malaria, resistance requires newer combinations of artemisinin with other therapies for effective treatment.