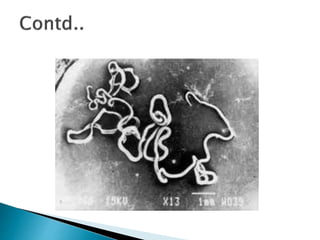
- Wuchereria bancrofti is a parasitic roundworm that causes lymphatic filariasis. It lives in the lymphatic vessels and lymph nodes of humans.
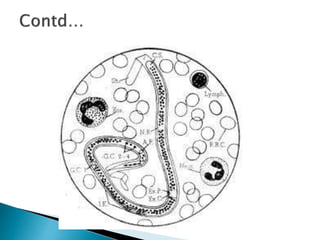
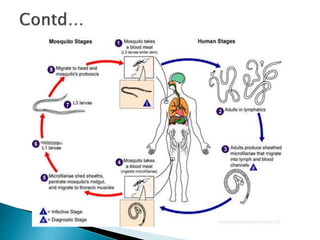
- The parasite has a two-host lifecycle, with humans as the definitive host and various mosquito species as the intermediate host. Microfilariae ingested by a mosquito develop into infective larvae that can be transmitted to another human.
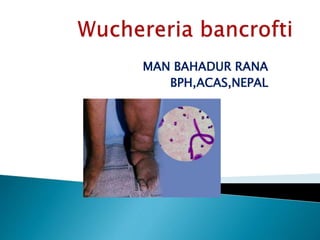
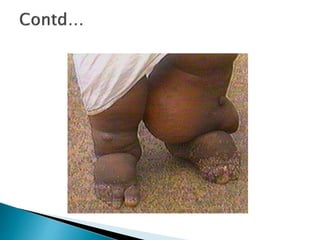
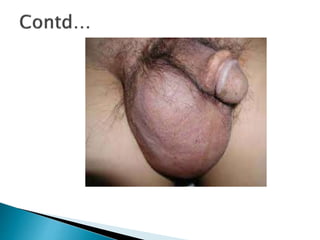
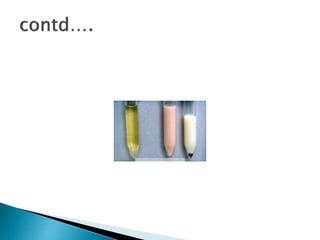
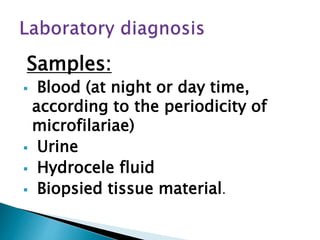
- In humans, adult worms cause lymphangitis and lymphadenitis, leading to symptoms like lymph edema, hydrocele, and elephantiasis. Occult filariasis involves high eosinophilia without microfilaremia. Diagnosis involves microfilariae detection in blood