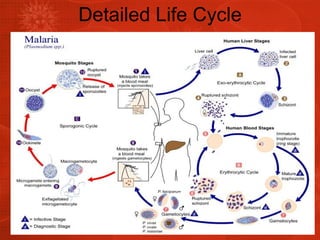
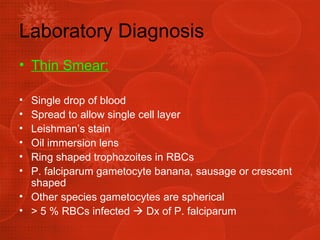
The document discusses Plasmodium, the parasite that causes malaria. It describes the different Plasmodium species that infect humans, including P. falciparum which causes the most severe form of malaria. The life cycle is explained, involving an asexual replication phase in humans and a sexual phase in mosquitos. Symptoms include fever, anemia, and enlarged spleen. Diagnosis involves examining blood smears under a microscope to identify the Plasmodium species and recommend treatment, usually chloroquine for sensitive strains.