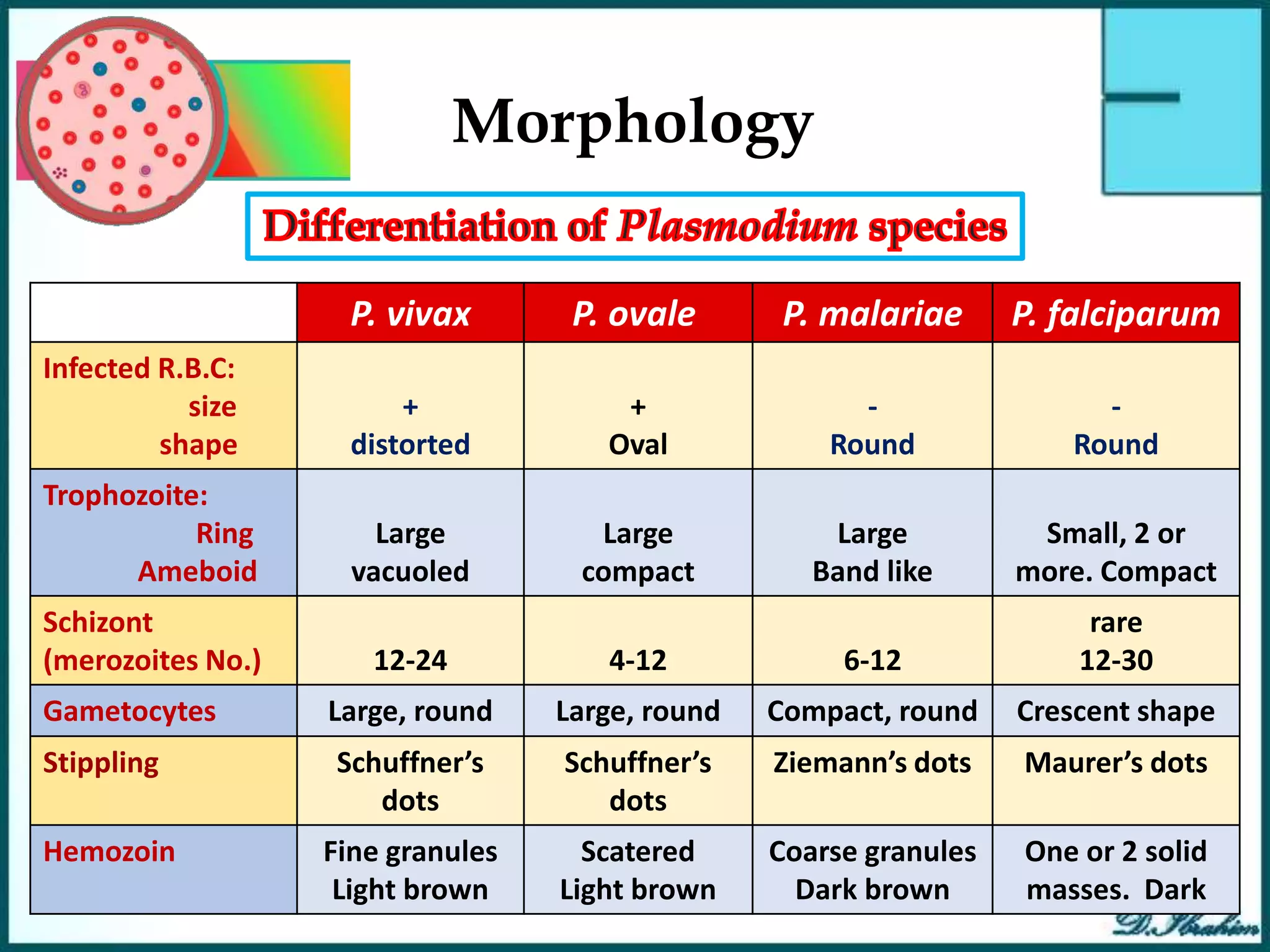
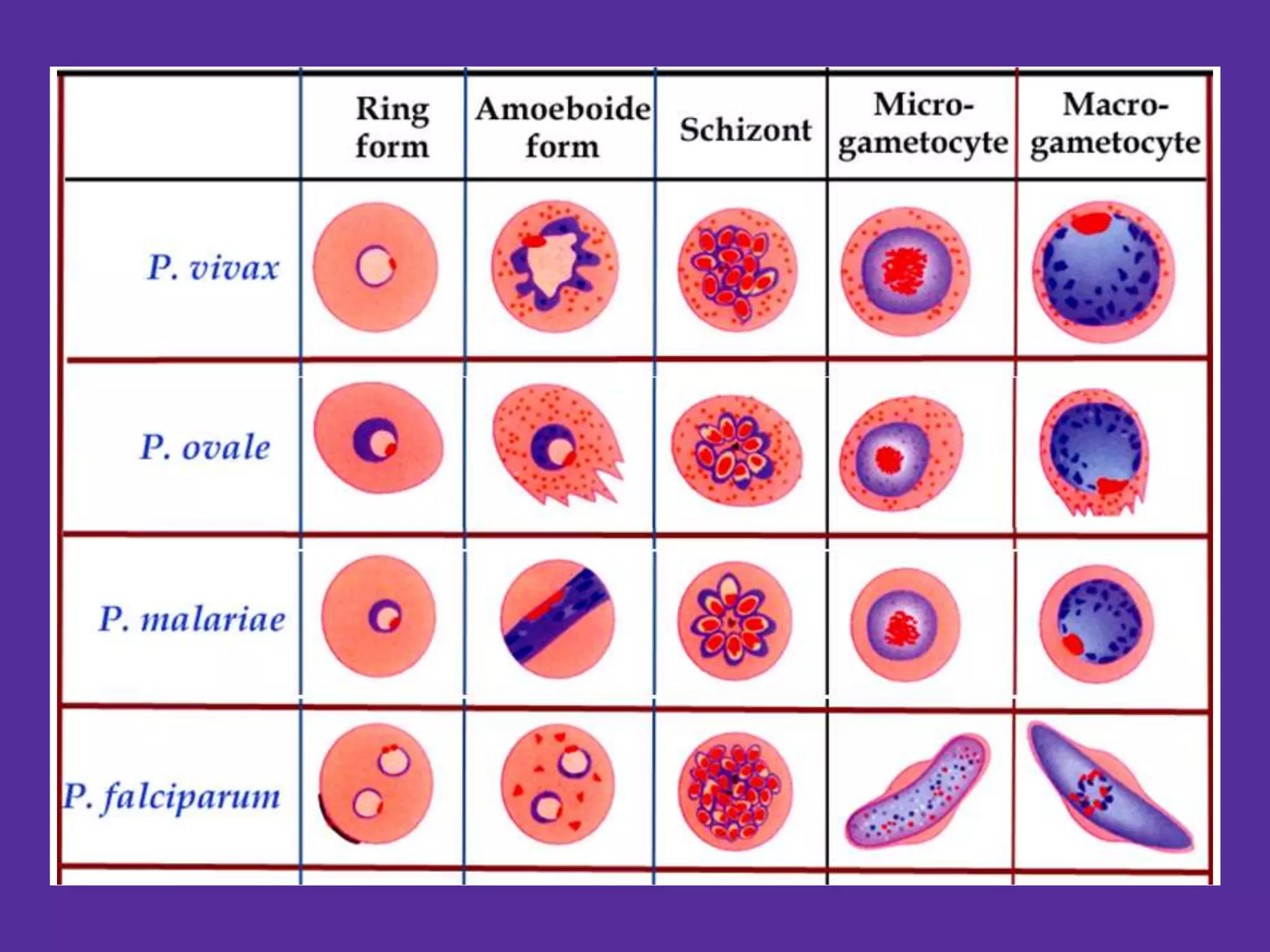
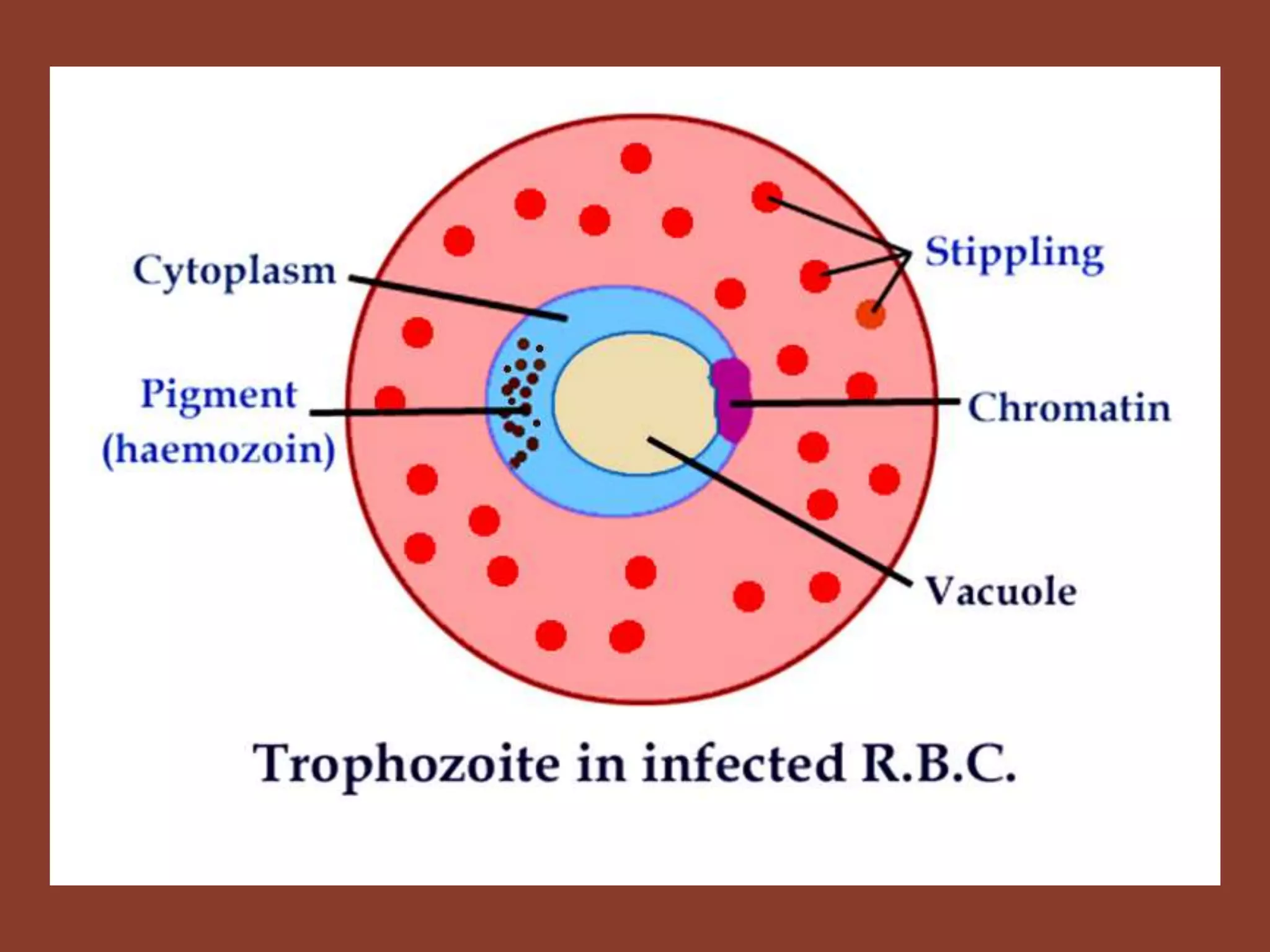
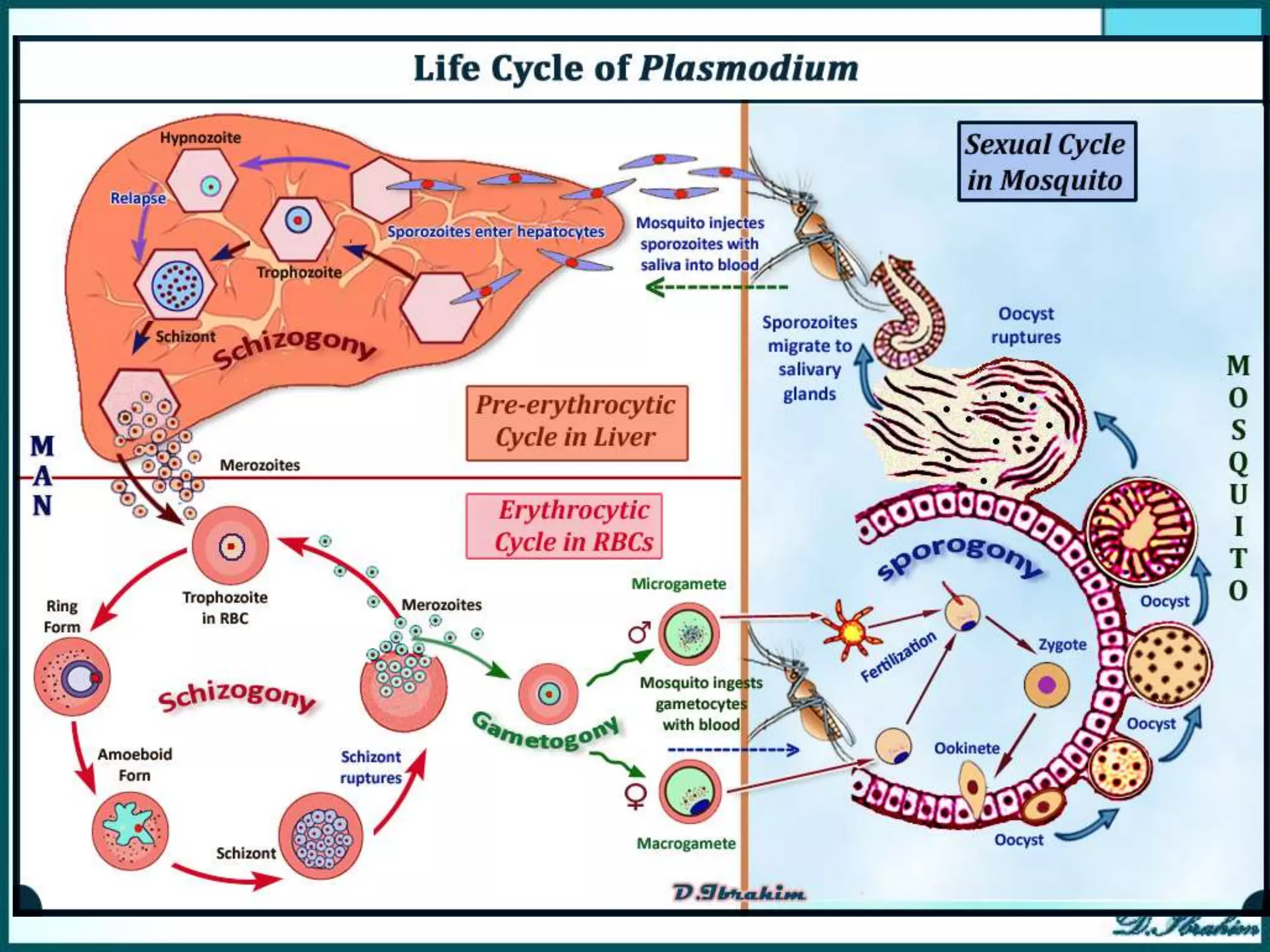
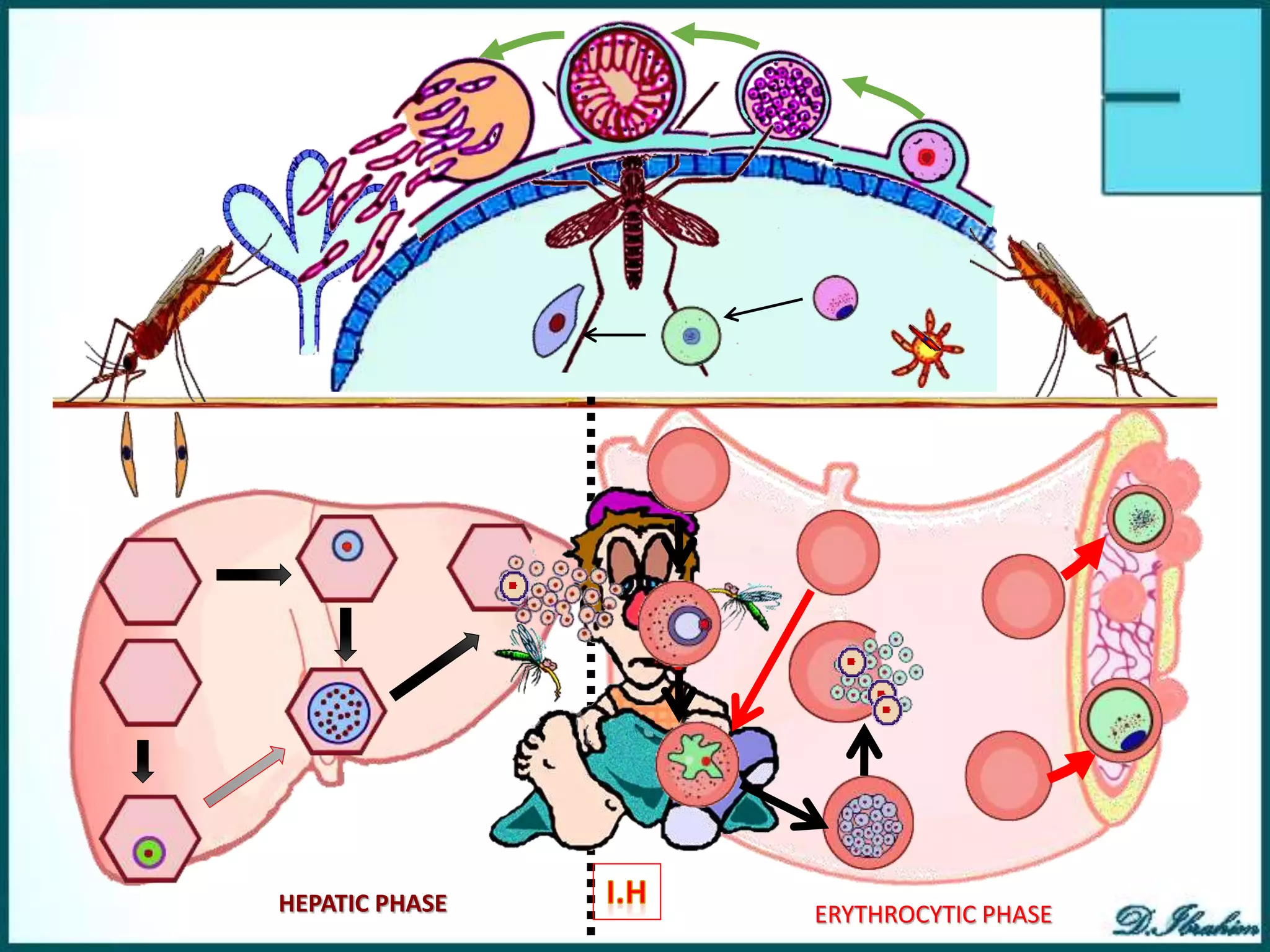
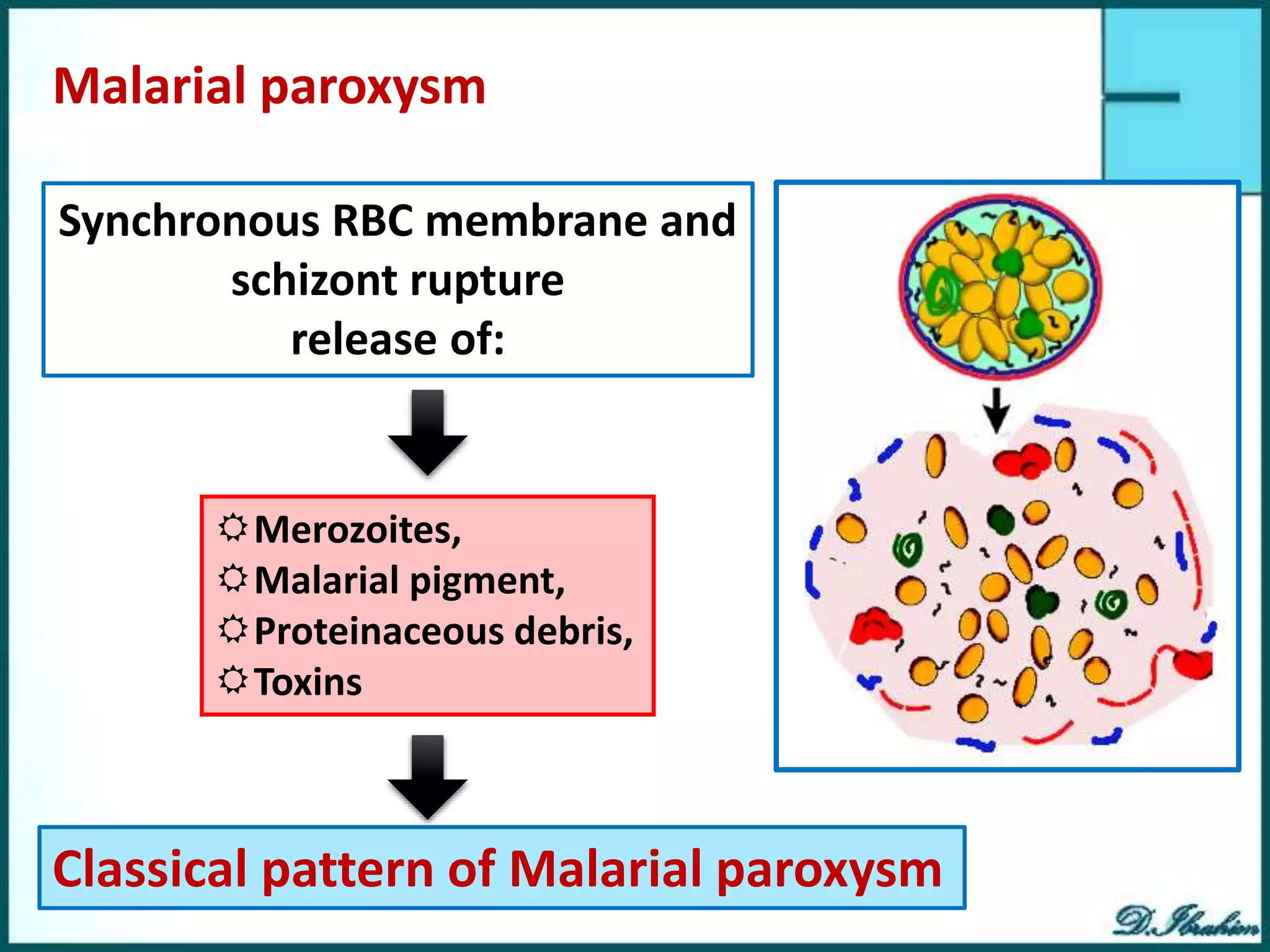
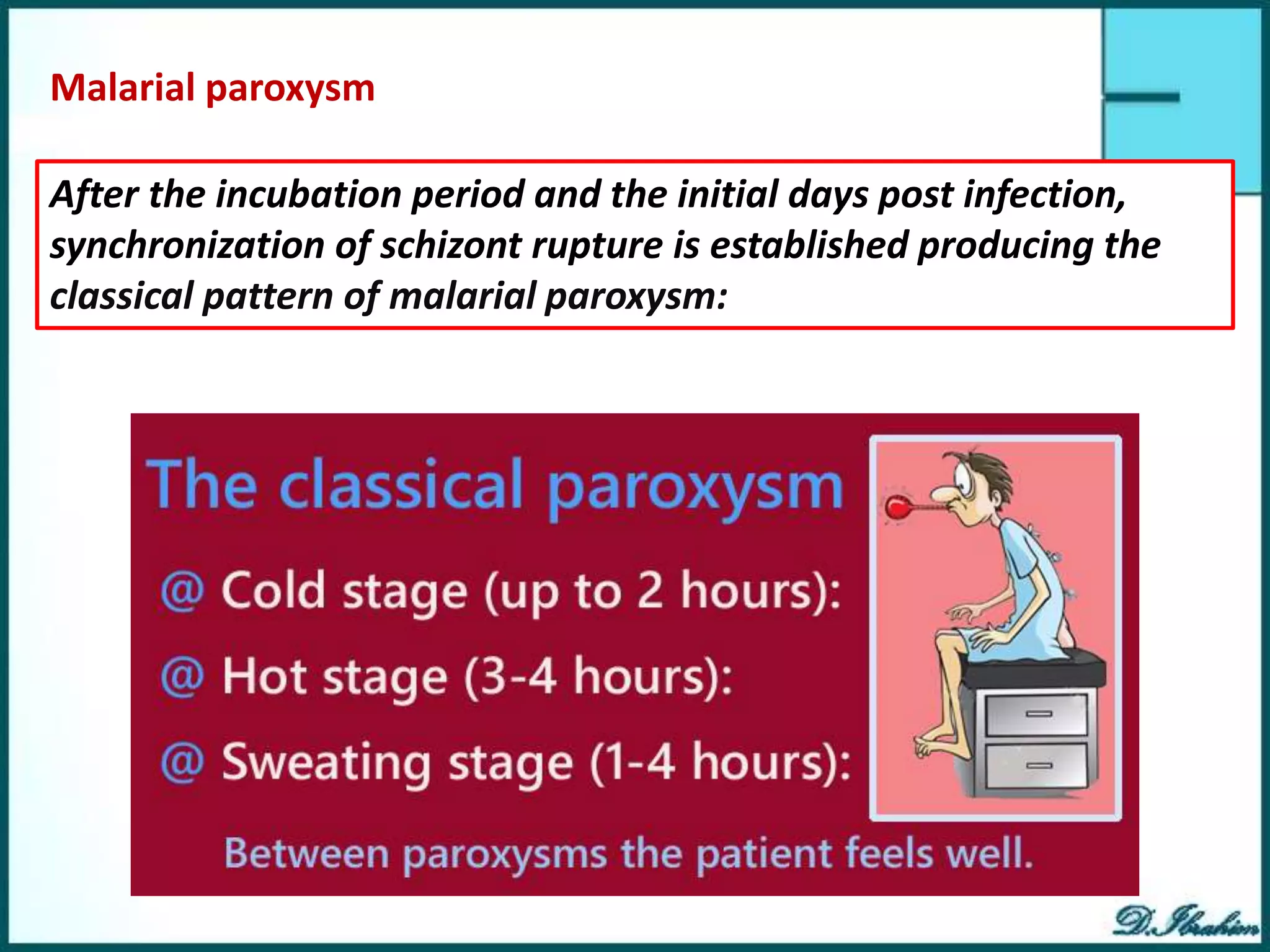
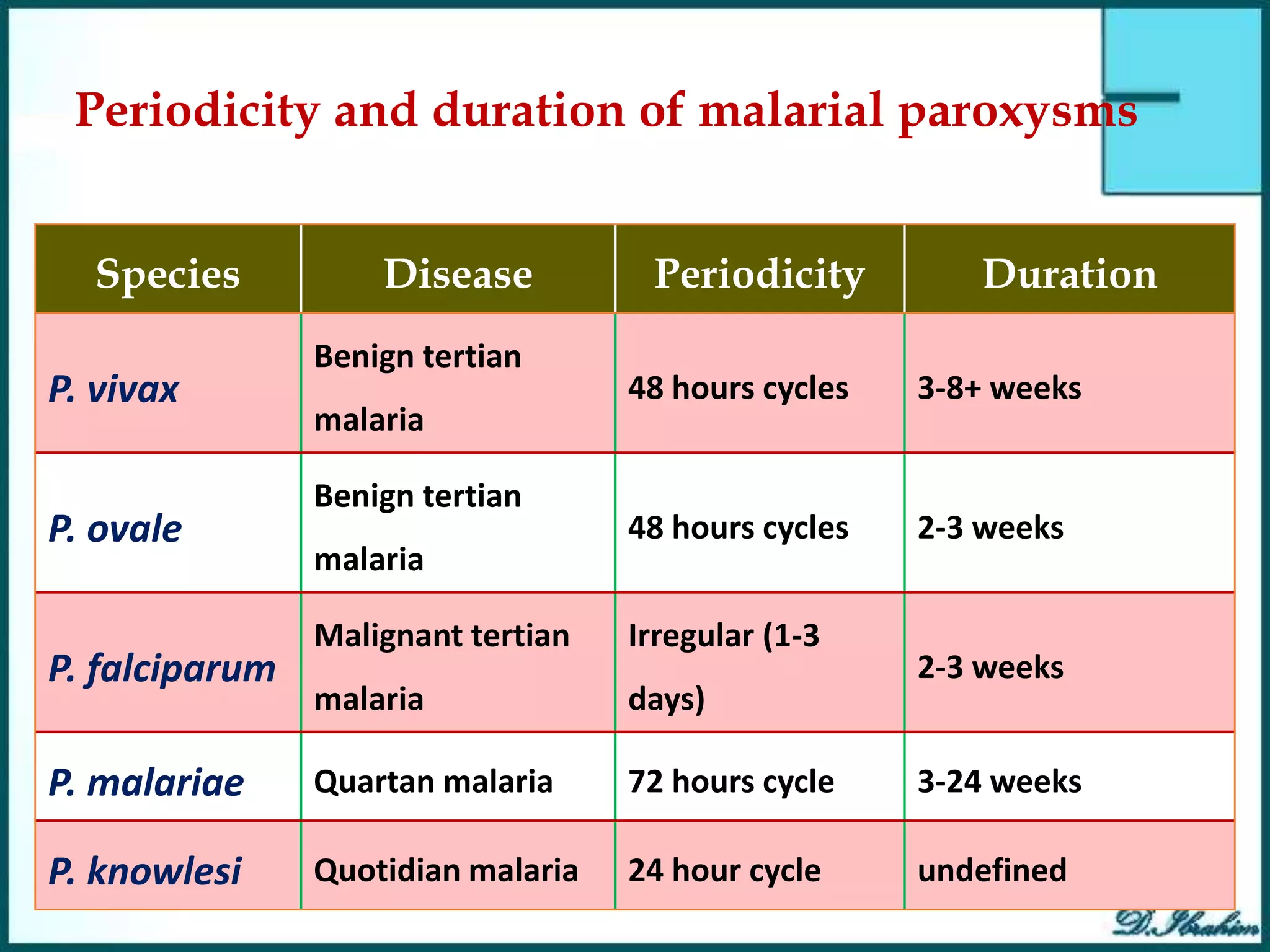
Malaria is caused by infection with Plasmodium parasites transmitted through the bites of infected Anopheles mosquitoes. There are five Plasmodium species that cause malaria in humans, with P. falciparum being the most deadly. The life cycle involves an initial hepatic phase followed by an erythrocytic phase where the parasites multiply within red blood cells. This causes cyclical fevers, chills, and other symptoms. P. falciparum malaria can progress to severe complications due to adhesion of infected cells and blockage of small blood vessels. Untreated malaria remains a major global health problem, especially among young children in sub-Saharan Africa.






























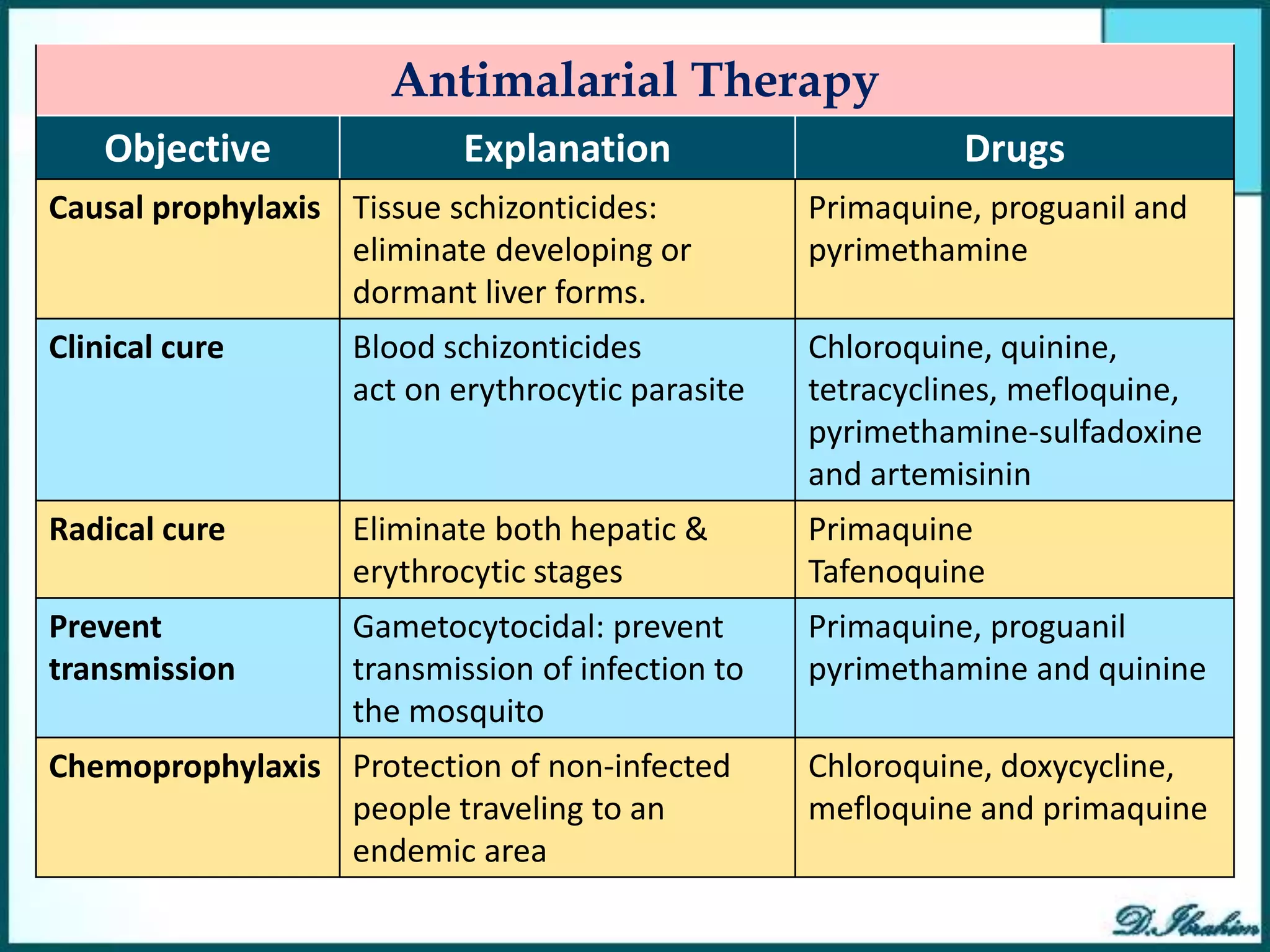
![chloroquine-sensitive malaria: Chloroquine phosphate; Dose: orally total dose 1.5
gm (10 tablets)
4 tablets [600 mg] initial dose.
2 tablets [300 mg] after 6 hours
2 tablets [300 mg] daily x 2 days
For prevention of relapses in vivax and ovale malaria, using primaquine 15mg /
day x 14 days to destroy hypnozoites in the liver.
Therapy of Uncomplicated malaria (P.
falciparum or species not identified):
chloroquine-resistant malaria:
A. Mefloquine: 15mg/kg in a single oral dose.
B. Combined chemotherapy is the best:
1) Quinine sulfate 650 mg tds x 3-7 days orally + one of the followings:
Doxycycline, Tetracycline or Clindamycin
2) Artemisinin-based combination therapy: Companion drugs with
Artemisinin in one tablet include lumefantrine, mefloquine, amodiaquine, or
sulfadoxine/pyrimethamine,
3) Atovaquone(250 mg )/ proguanil (100 mg) (Malarone®) 4 tabs qd x 3 days](https://image.slidesharecdn.com/plasmodiumspp-230727053539-5ffdb015/75/Plasmodium-spp-pptx-46-2048.jpg)




