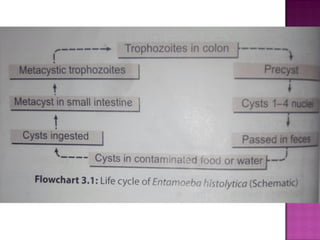
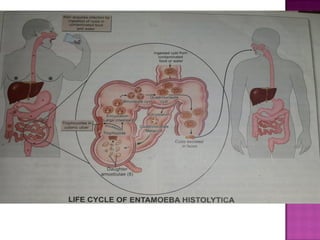
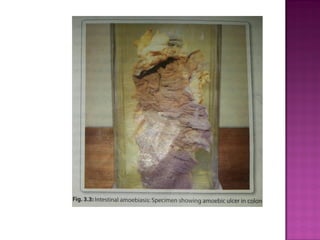
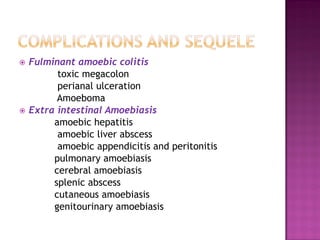
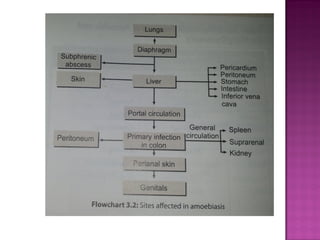
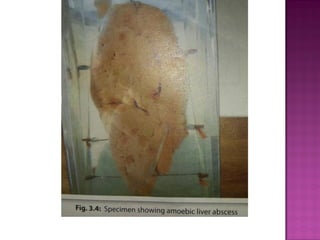
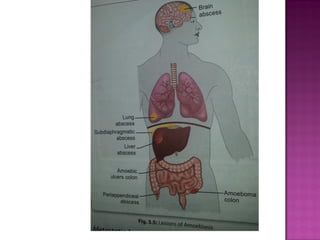
Amoeba are structurally simple protozoans that can invade and damage the intestinal tract. Entamoeba histolytica is an intestinal amoeba that can cause amoebic dysentery or form extra-intestinal abscesses in the liver and lungs. E. histolytica was first discovered in 1875 and exists in trophozoite, precyst, and cyst forms. The cyst form is infectious and can be transmitted through contaminated food or water. In the intestine, trophozoites may invade the colonic mucosa, causing ulcers or abscesses with symptoms of bloody diarrhea. Liver abscesses are a common extraintestinal manifestation and can spread infection to other organs.