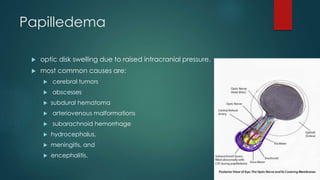
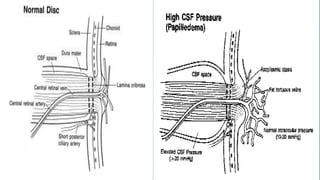
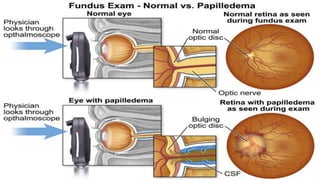
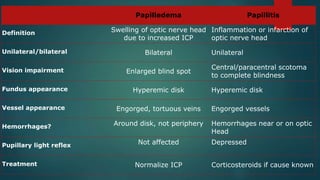
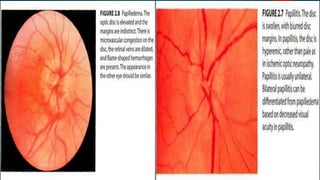
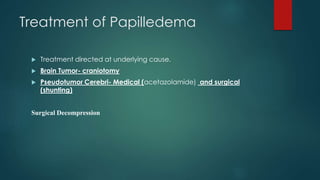
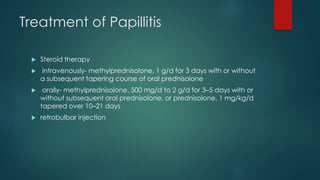
Papilledema and papillitis are two conditions that cause swelling of the optic disc. Papilledema is caused by increased intracranial pressure and results in bilateral swelling, while papillitis is caused by inflammation of the optic nerve and results in unilateral swelling. Key differences include papilledema causing an enlarged blind spot while papillitis causes vision loss, and papilledema showing engorged veins while papillitis can show hemorrhages. Treatment of papilledema involves treating the underlying cause of increased pressure, while papillitis is typically treated with corticosteroids.