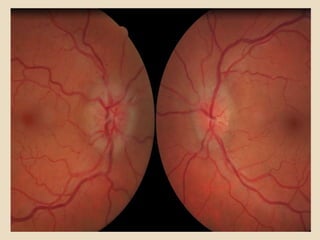
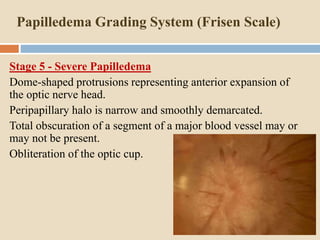
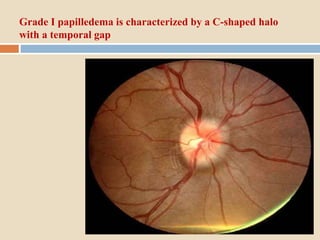
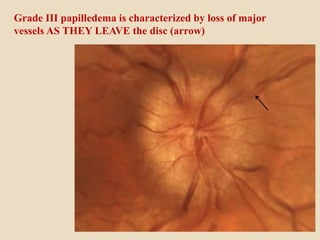
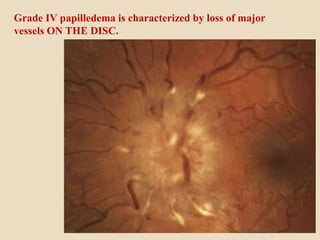
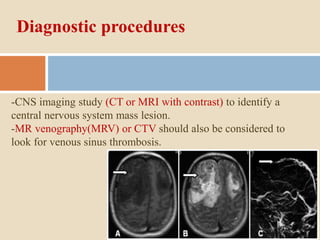
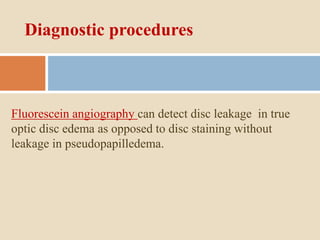
This document discusses papilloedema, which refers to optic disc swelling caused by increased intracranial pressure. It defines various types of optic disc swelling including unilateral, bilateral, and papilloedema. It also discusses pseudo-papilloedema. The causes, signs, symptoms, diagnostic workup, and grading scale of papilloedema are explained in detail. Treatment options for increased intracranial pressure including idiopathic intracranial hypertension involve medical management with carbonic anhydrase inhibitors and weight loss as well as potential surgical interventions.