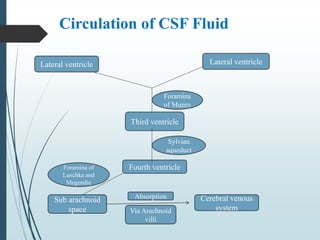
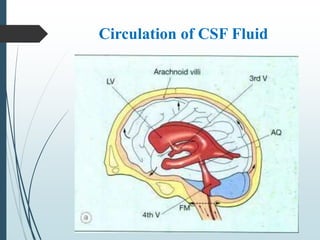
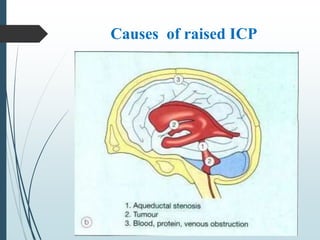
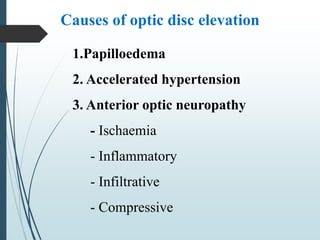
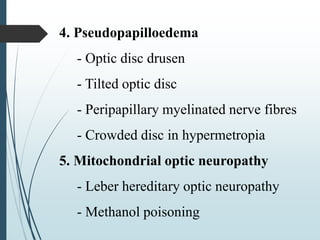
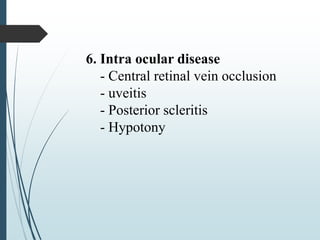
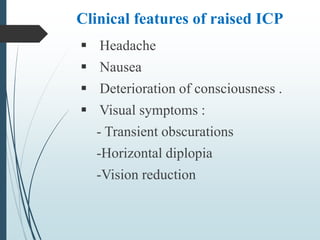
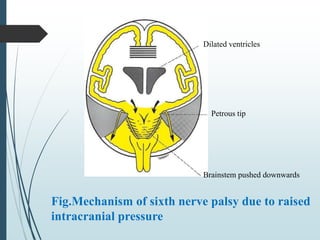
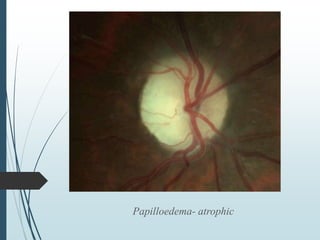
Papilloedema is swelling of the optic nerve head caused by increased intracranial pressure (ICP). It is nearly always bilateral and patients should be evaluated for an intracranial mass. Papilloedema can be caused by idiopathic intracranial hypertension, obstructive lesions, space occupying lesions, impaired CSF absorption, cerebral venous sinus thrombosis, cerebral edema from head trauma, or severe hypertension. Treatment involves reducing ICP through measures like mannitol infusion, CSF withdrawal, sedation, or surgery to remove masses. Complications can include visual loss or chronic headaches.