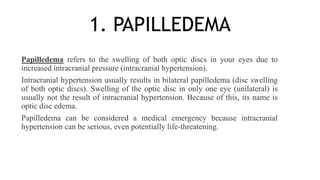
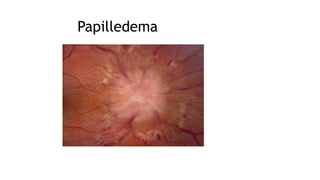
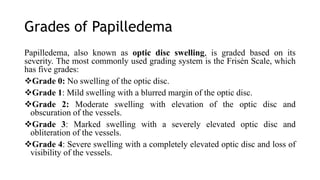
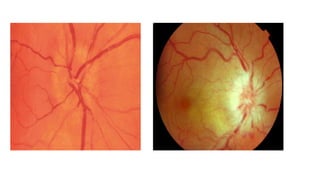
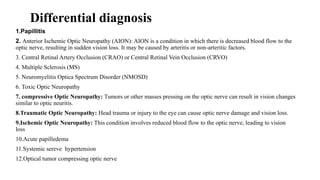
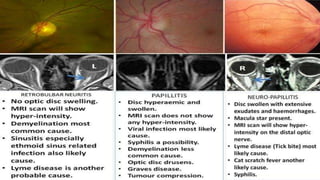
Papilledema refers to swelling of the optic discs due to increased intracranial pressure. If left untreated, it can cause vision loss or damage. Papillitis is inflammation of the optic nerve head, which can be caused by infections, autoimmune disorders, or other issues. It often causes reduced vision and color perception. Retrobulbar neuritis involves inflammation behind the eye affecting the optic nerve, and is a type of optic neuritis. It can be idiopathic or associated with conditions like multiple sclerosis.