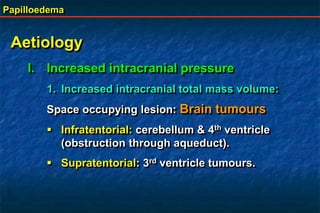
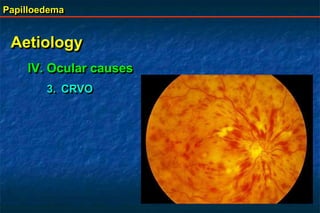
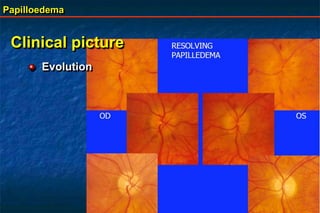
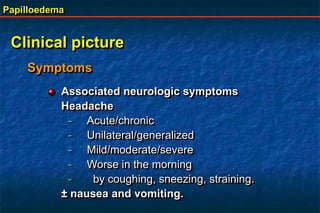
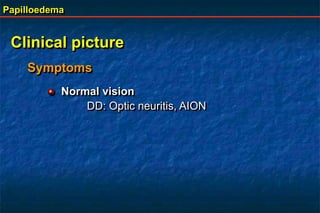
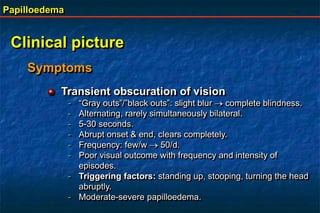
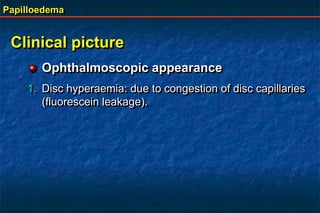
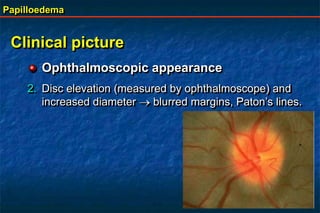
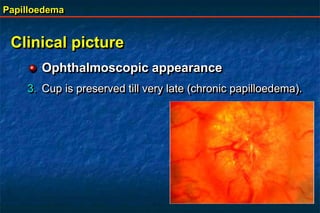
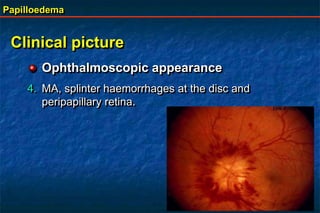
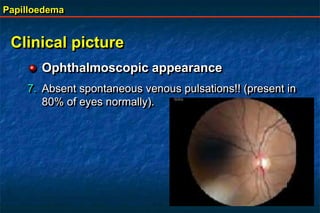
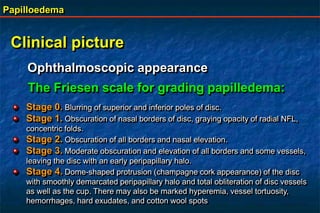
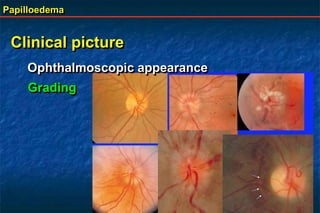
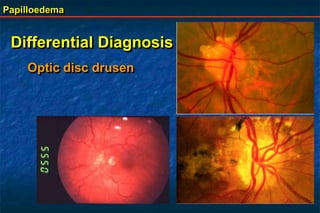
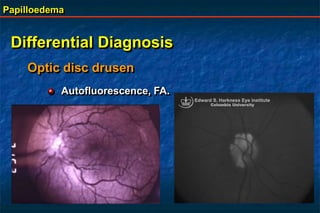
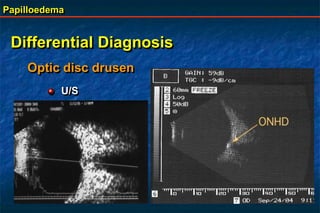
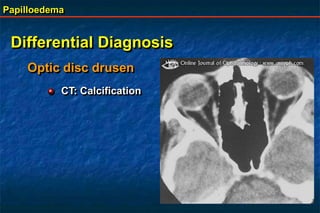
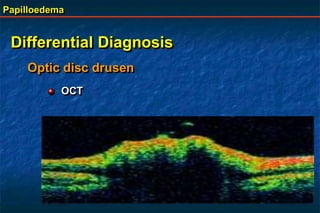
Papilloedema is swelling of the optic disc due to increased intracranial pressure. It is usually bilateral with normal vision. Common causes include brain tumors, subarachnoid hemorrhage, and idiopathic intracranial hypertension. On examination, papilloedema appears as blurred disc margins and venous engorgement. Grading scales are used to describe the degree of swelling. Differential diagnoses include papillitis, anterior ischemic optic neuropathy, and optic disc drusen.