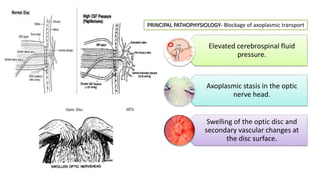
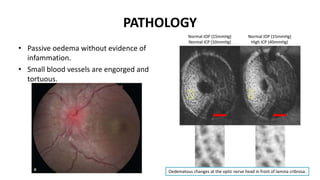
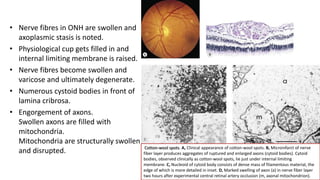
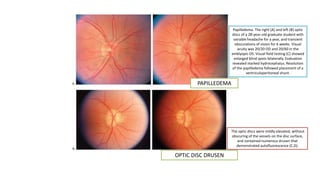
- Papilloedema is edema of the optic disc caused by increased intracranial pressure. It is a non-inflammatory condition where the optic nerve swells within the confined space of the optic nerve sheath.
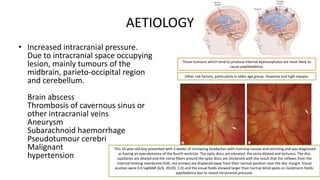
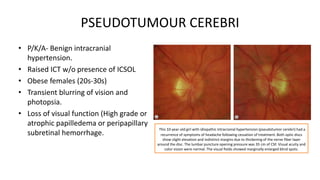
- Increased intracranial pressure from brain tumors, abscesses, venous thrombosis, aneurysms or pseudotumor cerebri can cause papilloedema.
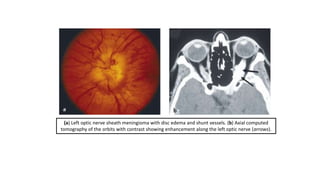
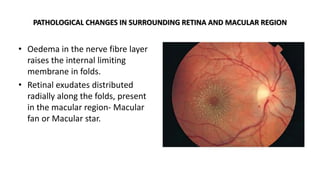
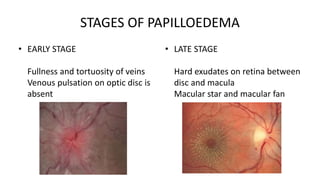
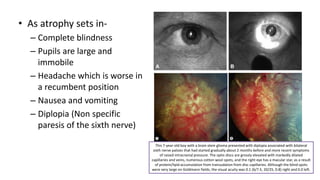
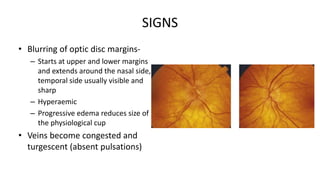
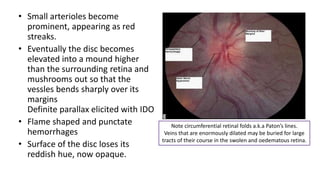
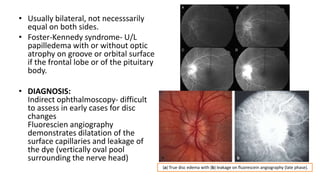
- On examination, the optic disc margins blur, the disc swells and veins become congested. Late stages show macular star/fan exudates and optic atrophy if untreated.
- Treatment is aimed at relieving intracranial pressure through tumor removal, shunting procedures or medication for pseud