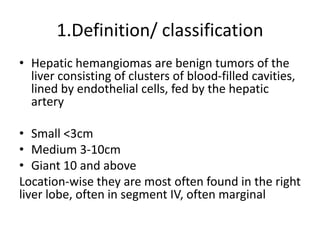
1) Hepatic hemangiomas are benign liver tumors consisting of blood-filled cavities lined by endothelial cells.
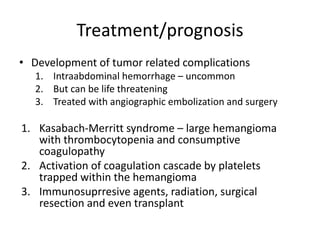
2) They are usually asymptomatic but can sometimes cause pain, nausea, or other digestive symptoms. Complications include bleeding, infection, or mass effect.
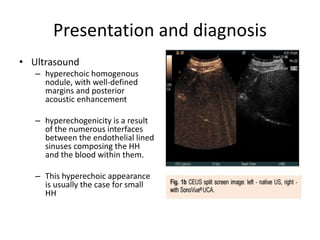
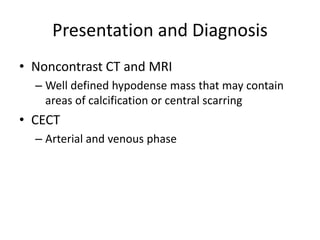
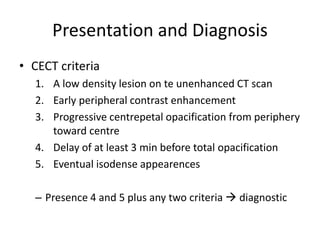
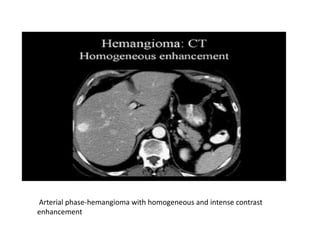
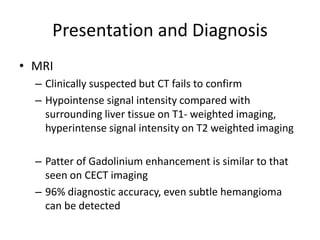
3) Diagnosis is usually made using ultrasound, CT, or MRI which show characteristic patterns of enhancement. Treatment is usually conservative but resection may be considered for large or symptomatic hemangiomas.