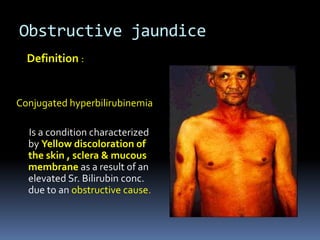
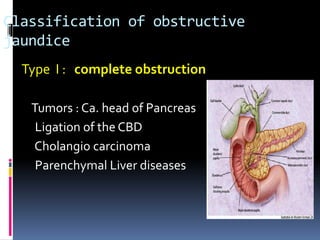
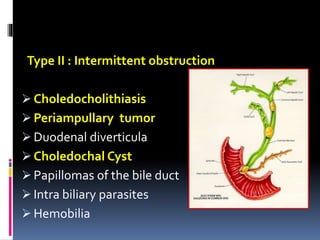
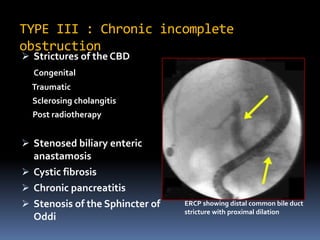
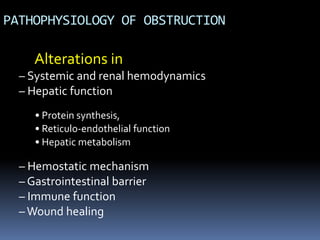
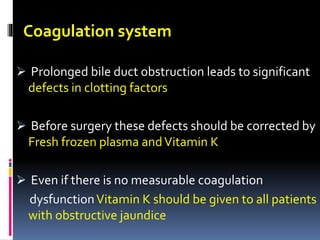
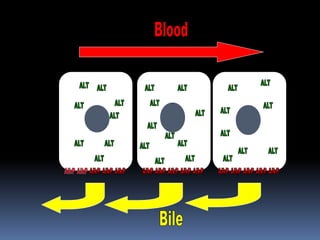
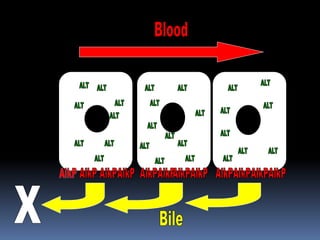
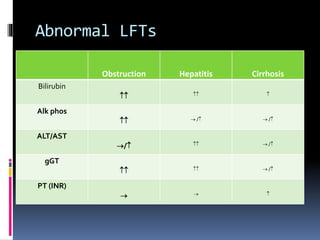
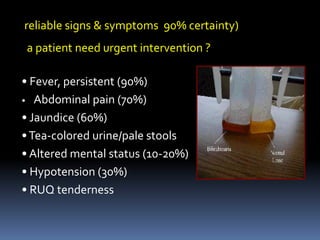
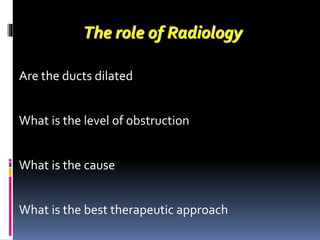
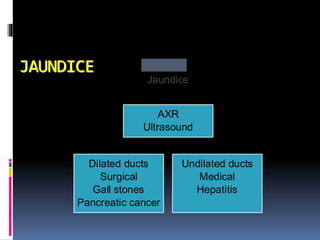
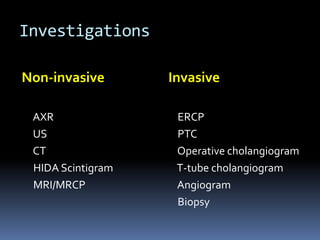
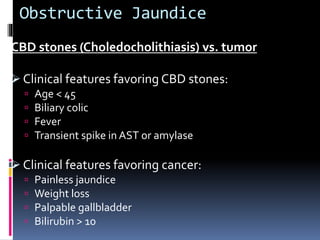
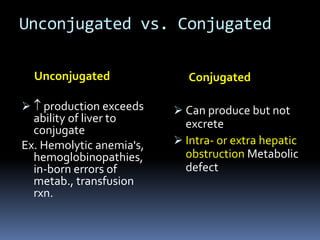
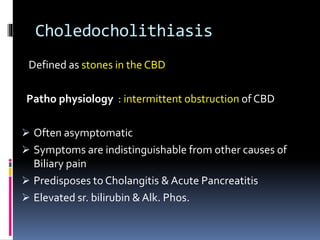
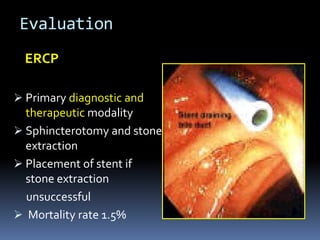
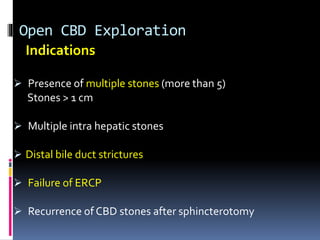
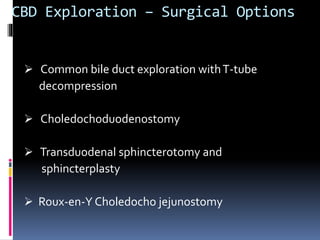
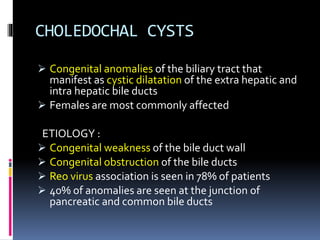
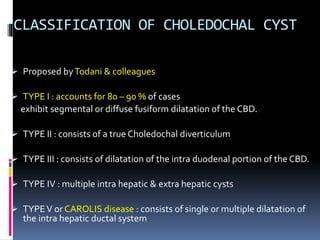
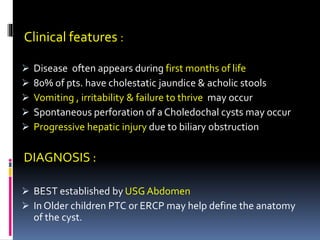
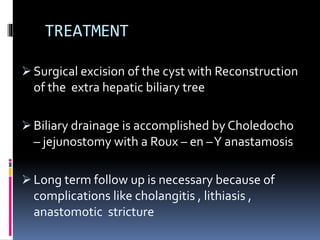
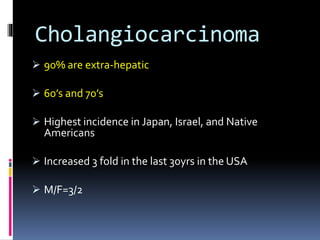
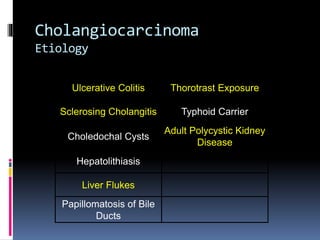
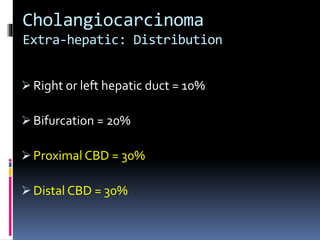
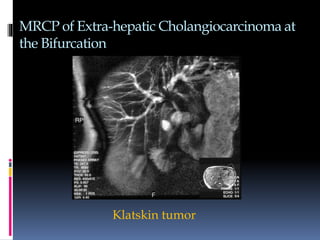
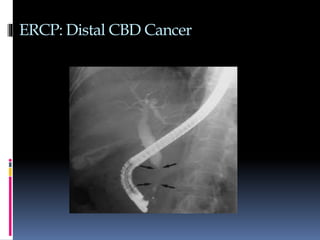
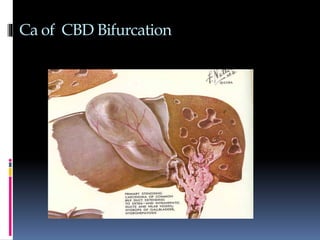
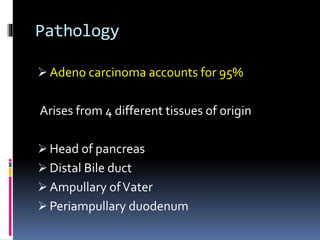
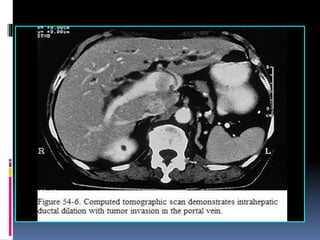
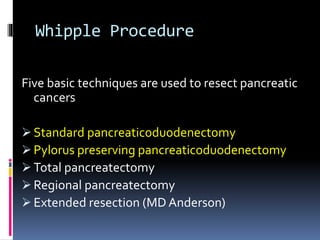
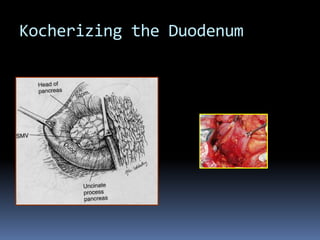
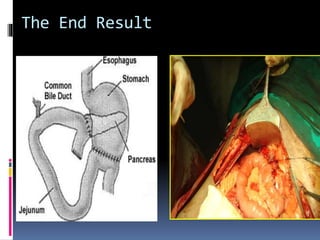
This document discusses obstructive jaundice, including its definition, classification, pathophysiology, signs and symptoms, investigations, and treatment. It covers four main types of obstructive jaundice - complete obstruction, intermittent obstruction, chronic incomplete obstruction, and segmental obstruction. Causes discussed include CBD stones, tumors, strictures, cysts, and parasites. The role of radiology, biomarkers, and surgery in evaluating and managing obstructive jaundice is also summarized.